The non-surgical option for vitreoretinal diseases
The non-surgical option for vitreoretinal diseases
--------------------------------------------------------------------------------
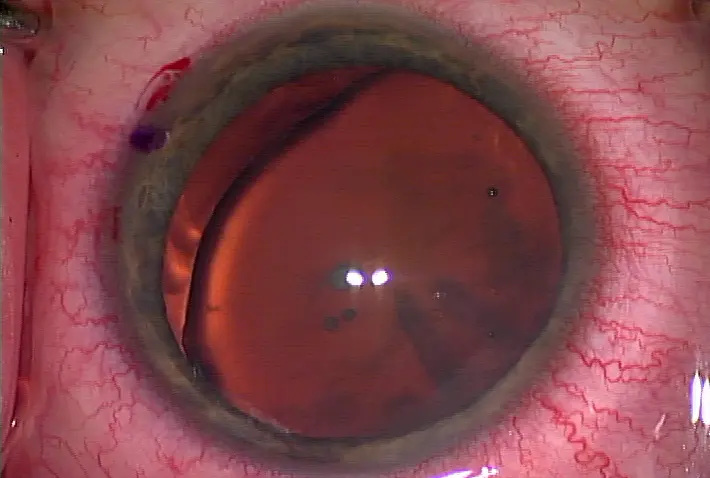
A graphic of the ocriplasmin molecule Source: ThromboGenics
A non-surgical treatment for symptomatic vitreomacular adhesion (VMA) including macular hole, vitreomacular traction syndrome (VMT), and epiretinal membrane (ERM) is now in the hands of the FDA. In April, ThromboGenics (Iselin, N.J.) submitted ocriplasmin for priority review by the agency, which could reach a decision on the drug by the end of the year. ThromboGenics is also pursuing European commercialization. Ocriplasmin could be available in Europe as early as October. "The product has been in development for eye diseases for about 5 years," said Ram Palanki, head of marketing, ThromboGenics. "We went through Phase I, II, and got our Phase III data in August of 2010. That's when we decided to go for the submissions in Europe and the U.S."
Ocriplasmin is a first-in-class small molecule delivered through an intravitreal injection that targets fibronectin, laminin, and type IV collagen fibers that adhere the vitreous to the retina. The goal is to create a clean separation of the posterior vitreous cortex and the inner limiting membrane of the retina, thus avoiding a vitrectomy and all the complications accompanying it. "With surgery things go wrong," said Keith Warren, M.D., chair, ophthalmology department, University of Kansas School of Medicine, Kansas City, on the importance of having a non-surgical treatment for vitreoretinal disease in ophthalmologists' armamentarium. "Every time you have an operation, you take a risk that something could go wrong. [The drug is] safer than surgery and less costly than surgery."
Clinical data results
More than 900 patients have been treated with ocriplasmin to date. The Phase III trial examined three distinct patient populations: those with VMT, those with ERM, and those with a macular hole. Patients either received a single injection of ocriplasmin or a single injection of saline. Resolution rates after the injection of both the drug and placebo were examined after 28 days. "If you pool the entire analysis and take the number based on an intend-to-treat population, 26.5% of the ocriplasmin-treated patients had resolution of VMA versus 10.1% with the placebo," said Dhaval B. Desai, senior product manager, ThromboGenics. Breaking out the numbers individually, though, ocriplasmin had a 29.8% resolution rate versus a 7.7% placebo resolution rate for the VMT group alone. ERM resolution rate was significantly smaller—8.7% for ocriplasmin compared with 1.5% for the placebo—but that "makes clinical sense," Mr. Desai said. "The thing to consider here is this was done in the era of time-domain OCT [optical coherence tomography]. In time-domain OCT it's hard to grade whether you have an ERM that's been hanging around, a very thick fibrotic kind of mess sitting there … or if it's [an] early cellophane maculopathy."
At 6 months, patients with a single dose of ocriplasmin saw a 40.0% closure rate of full-thickness macular holes compared with 17.0% in the placebo group. Furthermore, macular holes smaller than or equal to 250 microns had a 58.3% closure rate at 6 months with the drug. "The macular hole population is where some of the most striking data is," Mr. Desai said. "The important thing to note here is that the holes close early and they stay closed."
That's key, Mr. Desai said, because many macular hole patients fall into a watch-and-wait paradigm. "Doctors watch them hoping the VMA will release on its own, even though the historical data shows us that VMA will only release themselves 10% of the time," he said. "And there's no real way to predict any of that."
This is where ThromboGenics believes ocriplasmin will play a vital role. The 28-day resolution rate examination was not an accidental number. It's the average amount of time a patient with, for example, stage two macular hole has between diagnosis and a vitrectomy, Mr. Desai said. The thinking is that the patient can be diagnosed with the macular hole, be given an injection of ocriplasmin, and there's a possibility that the macular hole has resolved by the time the patient comes in for surgery.
"Now you've spared that patient a vitrectomy," Mr. Desai said.
Contraindications and side effects
The ThromboGenics team hasn't seen anything in regard to contraindications during the clinical trials, but certain population groups were excluded. High myopes at risk for retinal breaks and tears were omitted from the studies, as were patients who underwent a previous vitrectomy. Patients with retinal disease that could affect visual function or macular holes greater than 400 microns were also left out of the equation.
"Those holes tend to be hard to close even with surgery, so we wouldn't recommend using it on anyone with a macular hole greater than 400 microns," Mr. Desai said. Reported adverse events were minimal and centered around those occurring naturally during a VMA release including vitreous floaters and blurred vision.
Further research
Just because ocriplasmin is with the FDA doesn't mean ThromboGenics has finished its clinical studies. The company is currently examining ocriplasmin use for age-related macular degeneration and diabetic macular edema. Clinical results are not yet available. ThromboGenics is also looking into the safety profile of repeat doses of ocriplasmin. The company has some limited data currently, but it's not enough to make a judgment on widespread use. "I think this is going to change the spectrum of the disease," Mr. Palanki said. "[Physicians] probably won't see as many macular holes and probably won't see as many complications such as retinal detachments. I think this is going to alter the progression of a lot of vitreoretinal diseases as we start treating these patients."
Editors' note: Mr. Desai and Mr. Palanki are affiliated with ThromboGenics. Dr. Warren has no financial interests related to this article.
Contact information
Desai/Palanki: dhaval.desai@thrombogenics.com
Warren: kwarren@warrenretina.com
--------------------------------------------------------------------------------
by Faith A. Hayden EyeWorld Staff Writer
A graphic of the ocriplasmin molecule Source: ThromboGenics
A non-surgical treatment for symptomatic vitreomacular adhesion (VMA) including macular hole, vitreomacular traction syndrome (VMT), and epiretinal membrane (ERM) is now in the hands of the FDA. In April, ThromboGenics (Iselin, N.J.) submitted ocriplasmin for priority review by the agency, which could reach a decision on the drug by the end of the year. ThromboGenics is also pursuing European commercialization. Ocriplasmin could be available in Europe as early as October. "The product has been in development for eye diseases for about 5 years," said Ram Palanki, head of marketing, ThromboGenics. "We went through Phase I, II, and got our Phase III data in August of 2010. That's when we decided to go for the submissions in Europe and the U.S."
Ocriplasmin is a first-in-class small molecule delivered through an intravitreal injection that targets fibronectin, laminin, and type IV collagen fibers that adhere the vitreous to the retina. The goal is to create a clean separation of the posterior vitreous cortex and the inner limiting membrane of the retina, thus avoiding a vitrectomy and all the complications accompanying it. "With surgery things go wrong," said Keith Warren, M.D., chair, ophthalmology department, University of Kansas School of Medicine, Kansas City, on the importance of having a non-surgical treatment for vitreoretinal disease in ophthalmologists' armamentarium. "Every time you have an operation, you take a risk that something could go wrong. [The drug is] safer than surgery and less costly than surgery."
Clinical data results
More than 900 patients have been treated with ocriplasmin to date. The Phase III trial examined three distinct patient populations: those with VMT, those with ERM, and those with a macular hole. Patients either received a single injection of ocriplasmin or a single injection of saline. Resolution rates after the injection of both the drug and placebo were examined after 28 days. "If you pool the entire analysis and take the number based on an intend-to-treat population, 26.5% of the ocriplasmin-treated patients had resolution of VMA versus 10.1% with the placebo," said Dhaval B. Desai, senior product manager, ThromboGenics. Breaking out the numbers individually, though, ocriplasmin had a 29.8% resolution rate versus a 7.7% placebo resolution rate for the VMT group alone. ERM resolution rate was significantly smaller—8.7% for ocriplasmin compared with 1.5% for the placebo—but that "makes clinical sense," Mr. Desai said. "The thing to consider here is this was done in the era of time-domain OCT [optical coherence tomography]. In time-domain OCT it's hard to grade whether you have an ERM that's been hanging around, a very thick fibrotic kind of mess sitting there … or if it's [an] early cellophane maculopathy."
At 6 months, patients with a single dose of ocriplasmin saw a 40.0% closure rate of full-thickness macular holes compared with 17.0% in the placebo group. Furthermore, macular holes smaller than or equal to 250 microns had a 58.3% closure rate at 6 months with the drug. "The macular hole population is where some of the most striking data is," Mr. Desai said. "The important thing to note here is that the holes close early and they stay closed."
That's key, Mr. Desai said, because many macular hole patients fall into a watch-and-wait paradigm. "Doctors watch them hoping the VMA will release on its own, even though the historical data shows us that VMA will only release themselves 10% of the time," he said. "And there's no real way to predict any of that."
This is where ThromboGenics believes ocriplasmin will play a vital role. The 28-day resolution rate examination was not an accidental number. It's the average amount of time a patient with, for example, stage two macular hole has between diagnosis and a vitrectomy, Mr. Desai said. The thinking is that the patient can be diagnosed with the macular hole, be given an injection of ocriplasmin, and there's a possibility that the macular hole has resolved by the time the patient comes in for surgery.
"Now you've spared that patient a vitrectomy," Mr. Desai said.
Contraindications and side effects
The ThromboGenics team hasn't seen anything in regard to contraindications during the clinical trials, but certain population groups were excluded. High myopes at risk for retinal breaks and tears were omitted from the studies, as were patients who underwent a previous vitrectomy. Patients with retinal disease that could affect visual function or macular holes greater than 400 microns were also left out of the equation.
"Those holes tend to be hard to close even with surgery, so we wouldn't recommend using it on anyone with a macular hole greater than 400 microns," Mr. Desai said. Reported adverse events were minimal and centered around those occurring naturally during a VMA release including vitreous floaters and blurred vision.
Further research
Just because ocriplasmin is with the FDA doesn't mean ThromboGenics has finished its clinical studies. The company is currently examining ocriplasmin use for age-related macular degeneration and diabetic macular edema. Clinical results are not yet available. ThromboGenics is also looking into the safety profile of repeat doses of ocriplasmin. The company has some limited data currently, but it's not enough to make a judgment on widespread use. "I think this is going to change the spectrum of the disease," Mr. Palanki said. "[Physicians] probably won't see as many macular holes and probably won't see as many complications such as retinal detachments. I think this is going to alter the progression of a lot of vitreoretinal diseases as we start treating these patients."
Editors' note: Mr. Desai and Mr. Palanki are affiliated with ThromboGenics. Dr. Warren has no financial interests related to this article.
Contact information
Desai/Palanki: dhaval.desai@thrombogenics.com
Warren: kwarren@warrenretina.com



留言
張貼留言