Posterior capsulotomy: history of using the YAG laser and best practices
Posterior capsulotomy: history of using the
YAG laser and best practices
Alanna Nattis, DO SightMD
Babylon, New York
Robert Weinstock, MD
The Eye Institute of West Florida Largo, Florida
Stephen Weinstock, MD
The Eye Institute of West Florida Largo, Florida
JULY 2023 | EYEWORLD
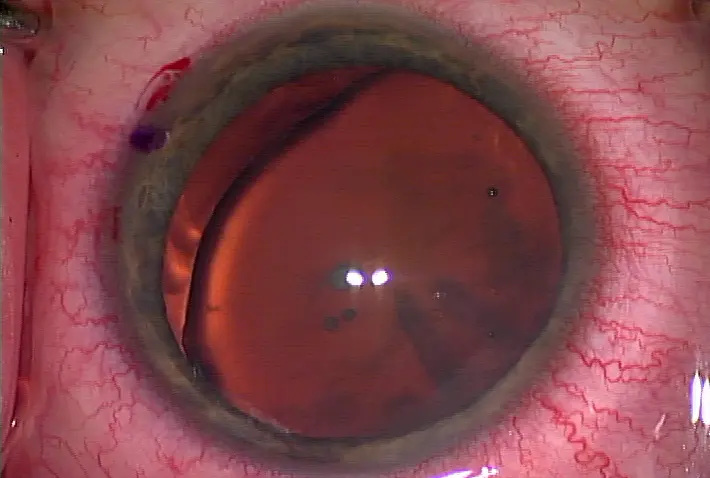
Following cataract surgery, patients may experience blurry vision. A posterior
capsulotomy with the YAG laser is often employed by physicians as a solution
to help patients achieve their desired vision. “A YAG capsulotomy has to be one of
the most commonly performed procedures for a cataract and refractive surgeon,” said
Robert Weinstock, MD. “Fortunately, it’s a safe, easy, and efficient technology.”
Prior to YAG capsulotomies and the invention of the YAG laser, this was a much more
challenging condition because it required going back into the eye and doing a surgical
procedure, with the risk of infection. In addition, when you rip the capsulotomy, it’s not
controlled, vitreous can come forward, and there can be PVD and retinal detachment, Dr.
Robert Weinstock said. “I think the YAG was one of the
greatest inventions in the history of ophthalmology,” he said. “It has made our lives so much
better having the technology.” Dr. Robert Weinstock noted that his father,
Stephen Weinstock, MD, was one of the first surgeons in the U.S. to have a YAG laser.
“When I started practicing 20 years ago, he taught me how to become an artist with the
YAG.” We’re trained to put this contact lens on the eye, use low power, and punch out the
capsule. “But for standard YAGs, [my father] taught me
that you don’t need to put a lens on the eye. You can use higher power and do a couple of
shots with the laser, and it splits it open without creating a big, punched out posterior
capsule that floats around in the vitreous,” he said. “We
use higher power with less shots now, which is much faster. … It’s become a much less
invasive procedure. This makes it more efficient and
takes only a couple of seconds.” Dr. Stephen Weinstock discussed his experience
with YAG, noting that he estimates around 30–40% of patients develop PCO and need a
YAG capsulotomy, no matter the precautions taken during surgery. It’s difficult to get 100%
of lens epithelial cells removed during a cataract procedure, he said.
Earlier YAG capsulotomies were more traumaticand less refined, he said. It wasn’t as
powerful or fine-tuned, and there were slightly more complications (the main complication
was lens dislocation into the vitreous). “Physicians were trying to figure out how to reduce
the need for posterior capsulotomy,” Dr. Stephen Weinstock said. “As the laser was refined,
I found that it was much easier to perform it with precision so that we could guide how
large of an opening we were going to create.” He said he’s seen very
few complications in the past 15–20 years. “Prior to that, when I was doing cataract
surgery, I used to spend a lot of time during the case vacuuming the posterior capsule,” he
said. “I started thinking it was foolish to do this when there are so few complications post-
YAG. “It used to be difficult when I would see a patient who had a posterior capsular
cataract because many of them did not come off the posterior capsule,” Dr. Stephen
Weinstock said. “They could require needling of the posterior capsule and/or a second
procedure, with a higher risk profile and worse outcomes. When the YAG was invented, it
was like a breath of fresh air because we didn’t have to worry about
going back into the eye. It was a paradigm shift in our approach to cataract surgery,” he
said. “I think this was one of the great advancements in surgery, and it led to other types of
lasers being developed for glaucoma and other conditions.” Alanna Nattis, DO, uses the
YAG laser frequently in her practice. “I do several per week, whether on my own patients
or those referred after having cataract surgery several years ago,”
she said. “It’s a successful and straightforward procedure for our patients and very
gratifying because it restores vision to what it was right after they had cataract surgery.”
She said the literature indicates that about 20–50% of patients will have PCO after surgery.
A lot of surgeons polish the posterior capsule, and that can help prevent PCO, but
sometimes it doesn’t, she said. “I like to explain to patients that it’s almost
like scar tissue has formed, and it can make the vision blurry. It can give them glare and
halos, and if that happens, we can do a laser procedure to help clear the central visual axis
again,” she said, adding that it only takes a few minutes to do the procedure, and she does
not use a contact lens with the YAG laser. “I aim the laser at the posterior capsule and try to
make a large symmetric opening in the central visual axis of the posterior capsule with as
little energy and as few shots as possible,” she said.
While the YAG laser procedure is not high risk, Dr. Nattis noted that there is a small risk of
retinal injury and retinal detachment. “That is not common today with the lasers that we
have, [but] I do always counsel my patients about that, especially in those who have had
prior retinal detachments.” Dr. Nattis said she doesn’t use a topical anesthetic because the
procedure is not painful, there’s nothing touching the eye when doing the procedure, and no
incisions are made. “I do tell the patients they will be blurry for 30–60 minutes or longer
after the laser, but by that evening or the next day, their vision will clear up significantly,”
she said. “I warn patients that it might make their floaters more noticeable.”
The techniques that have been developed to prevent opacification are great, Dr. Robert
Weinstock said. For example, the square-edge lenses are proven to reduce the migration of
lens epithelial cells, which are often the source of the opacification. Good cortical cleanup
with I/A and polishing of the capsule is another technique that can slow the process of
capsular opacification, he said. However, even with these options, the majority of patients
will ultimately need a YAG capsulotomy. There are some patients who have fibrosis
of the capsule itself during cataract surgery. Sometimes you can polish off some of the
opacity at the posterior capsule. Other times patients have had previous surgery, like retina
surgery, and there is scarring in the vitreous and postericontinued or plaques of fibrosis on
the capsule. Those can’t be removed at the time of cataract surgery, so those patients
require a YAG fairly quickly because once the cataract is gone and the new lens is in, it’s
cloudy, Dr. Robert Weinstock said. “I’m not a fan of doing a posterior capsulotomy at the
time of cataract surgery,” he said. “I think it introduces the potential for vitreous to come
through into the anterior segment, and the YAG is so safe and easy. In my opinion,
it’s easier to stage the procedures.” Dr. Robert Weinstock said that he will tell patients after
surgery that the capsule was opacified, and the safest move is to let the eye heal for
a month or so, then do the YAG capsulotomy. Dr. Robert Weinstock noted that a lot of
lenses in the premium cataract surgery arena are sensitive to PCO. The performance of
these lenses can be degraded by small amounts of PCO, whereas patients might not notice
as much with a monofocal. “Some surgeons are turning to earlier YAGs in the premium
IOL patients to improve the performance of the IOL,” he said. The other thing to note is
even with the best biometry and the best surgical technique, there are still cases of patients
who are off target after surgery. When these patients have paid for premium cataract
surgery, your goal is to get them out of glasses, and sometimes you must come back and do
a surface ablation to fine tune the vision. Dr. Robert Weinstock said he typically likes to do
the YAG capsulotomy first because there can be small changes of the refraction after the
YAG. “There can be minor changes to the lens position after you release some of the
tension on the posterior capsule,” he said. “In my mind, it’s best to do the YAG
capsulotomy first, let the eye heal for a couple weeks, then bring the patient
back, refract them, and move on to PRK or LASIK to fine tune the vision and reduce any
residual refractive error.”
For the routine YAG, it’s standard, he said. When you don’t put a contact lens on the eye,
you need more energy. The contact lenses focus the energy, and you need less energy. But if
you crank up the energy and don’t put the contact lens on, it’s just as effective, he
explained. “There are cases where we see contraction of the anterior capsule coming over
the optic, and sometimes it’s even squeezing the lens and causing it not to be in the right
location inside the eye,” he said. “If you use the YAG to make little nicks in
the anterior capsule, it can release the tension of the capsule and let the lens [settle into] a
more natural position.” Dr. Robert Weinstock cautioned against doing a YAG too early,
particularly in patients having problems with multifocals or EDOF lenses. The issue could
be neuroadaptation, he said, but some jump to doing a YAG early. The patient might end up
needing the lens explanted, depending on how they adapt, he said. “It’s a more
complicated capsulotomy has already been done by the laser because there is a continuation
of the eye to where the vitreous can come forward now that there is a hole in the posterior
capsule,” he said. Dr. Nattis recommended avoiding the YAG laser if the patient has a
cloudy cornea or if you don’t think you’re going to be able to perform the procedure
properly. Sometimes you can aim the laser beam so you can see the posterior capsule
tangentially and get around a small opacity at the cornea level, she said, but you want to be
sure you’re doing a complete procedure and not a partial YAG. Ultimately, these patients
with anterior segment haze or scarring may require a surgical capsulotomy if visualization
for a laser capsulotomy is poor. “We always check eye pressure before and after doing the
laser because in some patients, it can spike,” she added. Dr. Nattis said there’s no specific
timeframe within which to do a YAG; it’s when the patient becomes symptomatic. “We
tend to do YAG capsulotomies earlier in patients who have multifocal or trifocal IOLs
because those patients tend to be more sensitive to glare and halo,” she said.
While she doesn’t do surgical posterior capsulotomy often, Dr. Nattis said this might be
used for patients who can’t sit at the laser or who find it hard to maintain gaze in a certain
direction. Dr. Robert Weinstock said he performs surgical capsulotomy in rare situations. He
said he used this approach when he was doing a lot of Crystalens (Bausch + Lomb)
implantations because it was prone to capsular contractions, Z-syndrome, and major
displacements of the IOL where “you needed to do an IOL exchange and sometimes you
couldn’t do that exchange without some damage to the capsule, but you had to get the lens
out of there.” He said there are some situations with IOL exchange where the physician
might have to do a posterior capsulotomy with a vitrector to have a controlled
hole. This is usually avoided because the YAG laser is so easy and safe and is a much
more controlled procedure, he said. “One thing that I learned during residency
and in fellowship is sometimes it’s easy to miss a little thread of the posterior capsule that
might be still attached to the rest of the capsule that you’ve already lasered, and patients
may come back and say, ‘I still see something floating in my vision,’” Dr. Nattis said.
“Before I tell the patient the procedure is complete, I’ll do a once over to make sure there
are no posterior threads hanging on. You can go in and do a touch-up, but it’s good to save
yourself and the patient from doing that.”
Dr. Robert Weinstock discussed another way he uses the YAG laser. He said it can be used
for breaking up vitreous strands behind the capsule in the anterior vitreous.
It is a YAG laser, but the light focuses with that laser. “You can focus a little more
precisely into the vitreous. For people who suffer from anterior vitreous floaters that
are stuck in their vision and are causing haze, we do YAG laser vitreous photolysis,”
he said. That often helps a patient who suffers from bad floaters. “We will use the
YAG because of its optics to disrupt some of these fibrotic strands of vitreous that are
right in the vision, and it will break them up, much like you break up the capsule, then
gravity will help them drift out of the way,” he said. “We’ve had great success in avoiding
vitrectomies for floaters.”




留言
張貼留言