Using cataract surgery as a treatment for ocular hypertension
Using cataract surgery as a treatment for ocular hypertension
________________________________________
by Michelle Dalton EyeWorld Contributing Writer
James D. Brandt, M.D.
Steven L. Mansberger, M.D.
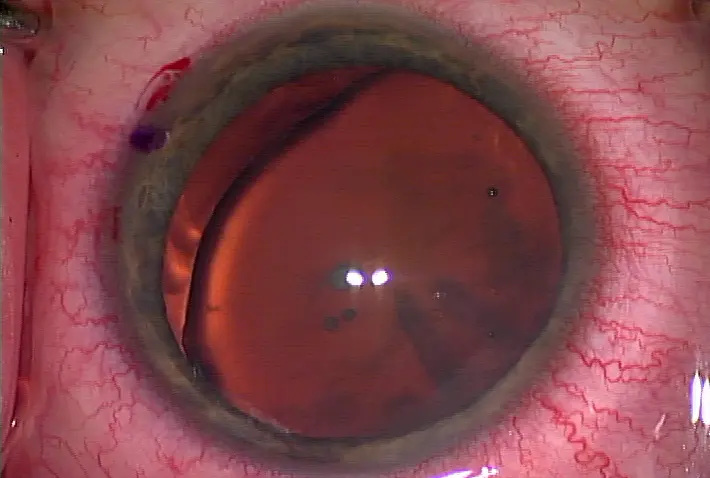
Cataract surgery can lower IOP in patients with ocular hypertension (OH), according to results from a large cohort study.1 Steven L. Mansberger, M.D., director, Glaucoma Services, Devers Eye Institute, Portland, Ore., and colleagues determined "someone who has early glaucoma or needs only 10-20% IOP lowering should be considered for cataract surgery," he said, but does stress the results are only applicable for those with OH, a point co-author James D. Brandt, M.D., professor of ophthalmology, and director, Glaucoma Service, University of California-Davis, reiterated.
"We only evaluated OH. It is dangerous to extrapolate the findings of this study to those with glaucoma. It's a whole different population, especially those on one or more meds," Dr. Brandt said.
The new study is "by far, the cleanest and best data available to date showing what happens when you remove a cataract from someone with elevated IOP," said Tom Samuelson, M.D., Minnesota Eye Consultants, Minneapolis. "When you remove a cataract from an eye with pressures elevated beyond traditional physiological levels, you are far more likely to see a reduction in pressure than when IOP is physiological pre-operatively."
In general, "ideas have been changing over the past few years" regarding cataract surgery's role in IOP management, said Leon W. Herndon, M.D., associate professor of ophthalmology, Duke University , Durham , N.C. 15 mm Hg. Very few studies have looked primarily at the effects of cataract surgery on IOP when the pre-surgical IOP was high. However, the literature is full of studies on this topic among patients with normal or near normal pre-op IOP. The effect of cataract removal on IOP in these two populations will be different."
Dr. Brandt said that the results are "probably the most accurate estimate of the average effect of cataract surgery in patients with elevated pressures," although he is careful not to suggest the results would be similar in moderate or severe glaucoma. Dr. Mansberger said for glaucoma patients "with early disease and cataract who require only a small decrease in IOP, I'll consider performing cataract surgery alone. Sometimes you'll be surprised how well controlled the IOP is after cataract surgery."
Not everyone will alter how he or she treats patients with elevated pressures, however. Dr. Mundorf noted he has not seen a "consistent lowering of IOP following cataract surgery" in his glaucoma patients and will continue to prescribe medications as a first-line therapy.
Patients with higher IOPs tended to have the greatest lowering effect post-cataract surgery, and Dr. Mansberger told EyeWorld "these patients may have a greater capacity to lower pressure after cataract surgery than those with normal tension glaucoma. For some reason, their trabecular meshwork isn't functioning as well. After surgery, the meshwork may provide more outflow facility for several reasons including opening the angle and stimulating the meshwork to work better."
Fitting cataract surgery into treatment regimens
By no means are the authors of the paper suggesting cataract surgery be a first-line treatment in all cases, but it should be considered, they said.
Dr. Mundorf will continue to offer medications as a first-line treatment, but "if a person has borderline IOPs and the primary complaint is related to cataract, I might proceed with the surgery and then re-evaluate the IOP to determine which path to take. I do believe I get more drop in IOP with a trabeculectomy than cataract surgery and more with the combination of cataract and trabeculectomy than cataract alone," he said. "I don't get any additional lowering, in the majority of my cases, by doing both the cataract and trab versus the trab alone."
Dr. Samuelson will offer cataract surgery as one option, but only if the patient has visual symptoms from the cataract. Otherwise, "I suggest using conservative means until they do have symptoms. I think medications and selective laser trabeculoplasty (SLT) are perfect for that purpose. When there's asymptomatic lens opacity, I favor buying time with medications and laser." In advanced glaucoma, however, "patients have far less optic nerve reserve, and we must be careful that we don't delay definitive treatment too long. We don't have the luxury to spend too much time on these more conservative measures," he said, and continues to recommend trabeculectomy in those instances.
If he's concerned about a conversion to primary open-angle glaucoma from ocular hypertension, Dr. Herndon said lasers—in particular, SLT—now get "more play in my practice." For patients with early glaucoma and who are treatment-naïve, "I'll immediately offer them the option of drops or SLT. Some studies have found SLT will be more cost effective in the long run for patients and for society. Now if the patient also has a little cataract, I won't hesitate to consider doing cataract surgery by itself," he said.
If patients are only marginally controlled on medication and want cataract surgery, Dr. Mundorf suggested proceeding with the surgery, and re-evaluating the level of IOP control gained around 6-8 weeks post-op before adding another medication, laser, or incisional surgery. Cataract surgery can, indeed, be a means of "giving patients with ocular hypertension or early glaucoma a drug holiday for a few years," Dr. Brandt said, but said most patients will need to be back on meds after that timeframe.
Discuss options with the patient, Dr. Mansberger said—if the patient doesn't mind the glaucoma drops, cataract surgery alone is viable. "Patients will tell you what they prefer, especially if they dislike the thought of being on glaucoma medications," he said. "The key thing in our paper, however, is that we did not randomize patients to cataract surgery. We can't compare if cataract surgery is better than laser or better than starting a drop on someone. And we can't take out a lens simply hoping for lower pressures—all of our patients had visually significant cataracts."
Once a patient has glaucoma, "that changes the indication for cataract surgery," Dr. Samuelson said. "I'm more likely to remove a cataract than perform trabeculectomy in patients with glaucoma and marginally or modestly uncontrolled intraocular pressure. This paper, and others like it, have caused us to play that cataract card earlier in the management of patients with elevated pressures."
Reference
1. Mansberger SL, Gordon MO, Jampel H, et al. for the Ocular Hypertension Treatment Study Group. Reduction in intraocular pressure after cataract extraction: the Ocular Hypertension Treatment Study. Ophthalmology. 2012;119:1826-31.
Editors' note: Dr. Brandt has financial interests with Alcon (Fort Worth, Texas) and MSD (Merck-Europe) and receives grant support from the National Eye Institute (NEI). Dr. Herndon has no financial interests related to this article. Dr. Mansberger has financial interests with Allergan (Irvine, Calif.) and Merck (Whitehouse Station, N.J.), and receives grant support from the NEI. Dr. Mundorf has no financial interests related to this article. Dr. Samuelson has financial interests with companies involved in micro-incisional glaucoma surgery.
Contact information
Brandt: jdbrandt@ucdavis.edu
Herndon: hernd012@duke.edu
Mansberger: smansberger@deverseye.org
Mundorf: tommundorf@aol.com
Samuelson: twsamuelson@mneye.com




留言
張貼留言