Challenging refractive cases Pharmaceutical corner Balancing risks and benefits
August 2010‧EyeWorld
by Vanessa Caceres EyeWorld Contributing Editor
Treating pregnant patients not an easy task Managing ophthalmic medications in pregnant patients is a challenging team effort between ophthalmologists and OB/GYNs, said Louis B. Cantor, M.D., Jay C. and Lucile L. Kahn Professor of Glaucoma Research and Education and vice chairman, Education, Department of Ophthalmology, Indiana University School of Medicine, Indianapolis.
"It's important to make decisions with the patient and their obstetrician," Dr. Cantor said.
Most specialists are vigilant about contacting patients' obstetricians as they want to protect the health of the mother and unborn baby and avoid dangerous side effects, said Jennifer R. Niebyl, M.D., professor and Residency Program Director, Department of Obstetrics and Gynecology, University of Iowa Hospitals and Clinics, Iowa City, Iowa. "They're scared to death of pregnant patients," she said.
Plus, although the U.S. Food and Drug Administration (FDA) has categories that indicate medication safety during pregnancy—A (safest), B, C, D, and X (highest potential risk)—many find these categories are not specific enough. For example, a medication may have a B or C rating not because it is proven unsafe but because there are no studies that show its risk to pregnant patients. Conversely, "just to say a medication is a B does not mean it is safe," Dr. Niebyl said.
Although the FDA announced in 2008 plans to update medication labeling with more specific written guidance about risk, these labeling changes have yet to occur.
Monitoring medication use in pregnant patients is probably a good idea for any physicians who are treating them—not only OB/GYNs. A study published online in November 2009 in the Journal of Maternal-Fetal & Neonatal Medicine found that two-fifths of OB/GYNs prescribed medication during pregnancy for which they did not have enough information about the potential effects on the unborn child. Additionally, "Nearly half reported that there are medical conditions for which they would like to prescribe medications but do not due to insufficient safety information," according to the study abstract. "These results indicate that [OB/GYNs] sometimes prescribe medications for pregnant patients under less than optimal conditions and emphasize the importance of generating up-to-date information on the effects of medications during pregnancy and having it readily available to health care providers," the investigators concluded. The study was led by the American College of Obstetricians and Gynecologists. Here's a rundown of how some ophthalmologists manage medications for common ophthalmic conditions in pregnant patients.
Glaucoma
Glaucoma might be the trickiest area for the treatment of pregnant patients. Nearly all glaucoma medications are in category C per the FDA. This means there are no good studies to show their effects in humans, although some animals treated with the medication had babies with problems. "No large studies have been done, and none of the drugs are 'proven' safe in pregnancy," Dr. Cantor said.
Take, for example, prostaglandin analogues. "Prostaglandins in large doses are used in obstetrics to induce labor or even abort a fetus, so there may be some concern using prostaglandin analogue eye drops, even though the dose level is very small," said Uday Devgan, M.D., chief of ophthalmology, Olive View-UCLA Medical Center, Sylmar, Calif.
For these reasons, Drs. Devgan and Cantor aim for a minimum amount of medication use during pregnancy; or, they aim to switch patients to other medication types.
Dr. Cantor evaluates how much the patient needs their glaucoma medications, their previous pregnancy history, and the results of discussions with the patient's obstetrician. "I've had more women who have opted to discontinue their medications during pregnancy," he said. "A few months of a gap in their therapy does not usually result in a substantial change in their visual status."
Dr. Cantor tries to change his expectations for pregnant patients. So, for instance, if their IOP was 15 or 16 mmHg with therapy and it goes to 30 mmHg without therapy, he may try to lower it to 24 mm Hg on minimal therapy during pregnancy. It also works in some patients' favor that their IOP naturally lowers during pregnancy, he added.
If he decides that a patient should and can continue their medications, he will lower the dosage. He may prescribe a beta blocker like timolol (various manufacturers), but instead of a 0.5% dose twice a day, he will prescribe 0.25% once a day. He will also take a similar lowering approach with brimonidine, prescribing a 0.1% dose (Alphagan P, Allergan, Irvine, Calif.). Brimonidine is a category B drug.
Dr. Cantor also discusses the option of laser trabeculoplasty, a surgical approach that may not help for more than 3-5 months, but that may just long enough to get patients through their delivery, he said.
When instilling eye medications during pregnancy, Dr. Cantor recommends that patients put in their drops, close their eyes, and sit still for a few minutes, instead of blinking. This reduces systemic absorption, he said.
Dry eye
Although hormone fluctuations seem to make dry eye more common in pregnant patients, the exact cause and effect isn't clear, said Robert Latkany, M.D., founder and director, Dry Eye Clinic, New York Eye and Ear Infirmary, New York. Additionally, he's spoken with patients who had dry eye and then found, curiously, their symptoms alleviated during pregnancy, he said.
Like other ophthalmologists, Dr. Latkany favors a minimalist approach. "If the problem is not sight-threatening and not in the extreme category, I keep medication to a minimum," he said. He might usually start a non-pregnant mild dry-eye patient with Restasis (cyclosporine ophthalmic emulsion, Allergan, Irvine, Calif.), but he steers pregnant patients away from that until after delivery. If the patient has symptoms that are making them miserable or are causing abrasions, Dr. Latkany will call the patient's obstetrician to confirm that any medication used is acceptable.
One common form of relief in pregnant patients with dry eye is punctal plugs—most patients like them and keep them in even after they deliver, Dr. Latkany said. There are a few who have them removed afterward only because they get too many tears. "But the majority prefer the extra moisture," he said.
General eye health
No matter what their problem during pregnancy, ophthalmologists suggest that patients try and minimize systemic absorption of their eye medications. In fact, Christopher J. Rapuano, M.D., professor of ophthalmology, Jefferson Medical College, Thomas Jefferson University, Philadelphia, and co-director, Cornea Service, Wills Eye Institute, Philadelphia, teaches patients digital punctal occlusion. "This is how to press their finger between their eye and their nose to close their tear drainage ducts just before and for one minute after eye drops are instilled," Dr. Rapuano said. "This simple maneuver decreases the systemic absorption of eye drops significantly."
Dr. Rapuano prefers to avoid medications during pregnancy, but in the occasional times when meds must be used, he will consult with the obstetrician and teach the patient digital punctal occlusion. "Or, I actually place silicone punctal plugs in the tear ducts, which impedes the drops getting into the circulation and to the fetus," he said.
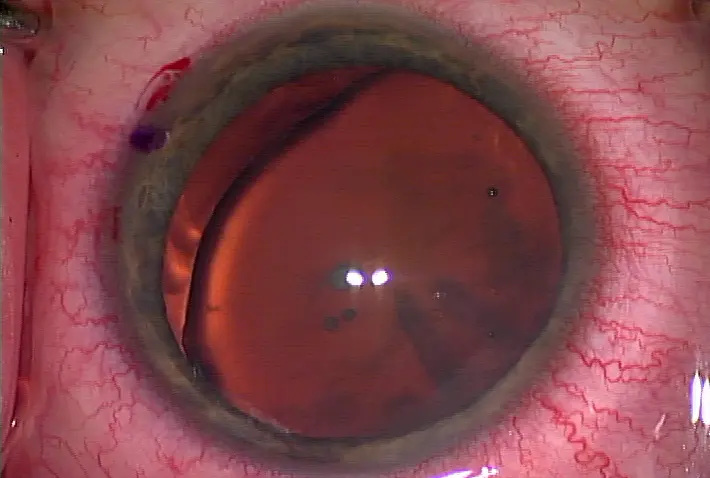
Dilation is another area that is typically avoided during pregnancy, Dr. Devgan said. "When we treat newborns and infants, we cannot use our usual dilating drops since these can be absorbed and get into their system, where they can have many side effects," he said. "There are special lower concentrations of these drops that are used for babies. The same applies to pregnant patients since the sympathomimetic drops (phenylephrine) and anti-cholinergic drops (such as atropine) can affect the babies."
Ophthalmologists also spend some time educating patients about common eye occurrences during pregnancy (see sidebar geared toward patients)—they may find their glasses and contact lenses not fitting as well due to refractive changes. Plus, they may not want to take care of their eyes as well due to exhaustion. Dr. Latkany sees more pregnant patients sleeping in their contacts during pregnancy because they are so tired. He also has observed anecdotally more patients experiencing floaters during pregnancy.
All physicians may want to use their time with pregnant patients to review other healthy habits. While OB/GYN Dr. Niebyl said it is common to discuss medication use with this population group, it's easy to forget to ask about cigarette and alcohol use, which are probably more common and could be more harmful. "You have a patient who comes in and asks about taking a benign drug, but then you find out she smokes a pack a day. That puts things in perspective," she said.
Editors' note: Dr. Cantor has financial interests with Alcon (Fort Worth, Texas), Allergan (Irvine, Calif.), Merck (Whitehouse Station, N.J.), Pfizer (New York), and QLT Therapeutics (Vancouver, British Columbia). Dr. Niebyl has no financial interests related to her comments. Dr. Devgan has financial interests with Abbott Medical Optics (Santa Ana, Calif.), Alcon, and Staar Surgical (Monrovia, Calif.). Dr. Latkany has financial interests with Alcon and Allergan. Dr. Rapuano has financial interests with Alcon, Allergan, and Bausch & Lomb (Rochester, N.Y.), among other ophthalmic companies.
Contact information
Cantor: 317-274-8485, lcantor@iupui.edu
Devgan: devgan@ucla.edu
Latkany: 212-832-2020, relief@dryeyedoctor.com
Niebyl: 319-384-9247, jennifer-niebyl@uiowa.edu
Rapuano: 215-928-3180, cjrapuano@willseye.org
For patients: eye health and your pregnancy
1. Your vision may change during pregnancy. This could mean that your glasses or contact lenses don't work as well. For this reason, refractive surgery is not recommended during pregnancy. Your vision should return to normal after pregnancy 2. Be prepared to use your glasses more often. In addition to vision changes, the shape of your cornea often changes during pregnancy, making your contact lenses not fit as well. A good pair of glasses will come in handy for those middle-of-the-night feedings 3. Remember to take out your contacts before you go to sleep. Although pregnancy can be an exhausting, it is more important now than ever to take good care of your eyes. Sleeping with your contacts on can increase the risk for eye discomfort and infection 4. Tell your ophthalmologist about any medications you are using. He or she will discuss with you and your obstetrician whether you need to continue to use eye medicines during pregnancy. Most ophthalmologists aim for minimum use—if any use—of drugs during pregnancy 5. If your ophthalmologist decides you must continue to use certain eye medications, he or she will teach you a way to keep the medicine only in the eye and minimize the amount of medicine that reaches that rest of your body 6. If you are nursing once the baby is born, your ophthalmologist may continue to monitor what medicines you use 7. For more information about medication use during pregnancy, visit the following website from the U.S. Department of Health and Human Services: www.womenshealth.gov/faq/pregnancy-medicines.cfm




留言
張貼留言