Measurement remains key to best toric IOL outcomes
Toric IOLs
Measurement remains key to best toric IOL outcomes
by Rich Daly EyeWorld
Contributing Writer
"Despite all this planning and preparation, one can still have uncontrollable intangibles and end up with residual, off-axis astigmatism. Just be prepared to handle these eventualities postoperatively …"
– Sydney L. Tyson, MD |
Although many patients
can benefit from toric lenses, surgeons have to take special care to ensure
their fit and location
Adhering to key measurement
steps in toric lens implantation can keep both standard and challenging
astigmatism patients on track.
Although Sydney L. Tyson, MD, an attending surgeon atWills
Eye Hospital ,
Philadelphia
"In general, I believe that maximizing the treatment of regular astigmatism will greatly improve these patients' overall vision even if there is some residual irregular astigmatism," Dr. Tyson said. "I do make sure to inform the patient of this reality."
Audrey Talley Rostov, MD, in private practice,Seattle
Although Sydney L. Tyson, MD, an attending surgeon at
"In general, I believe that maximizing the treatment of regular astigmatism will greatly improve these patients' overall vision even if there is some residual irregular astigmatism," Dr. Tyson said. "I do make sure to inform the patient of this reality."
Audrey Talley Rostov, MD, in private practice,
Preop prep
For Dr. Talley Rostov the key to a successful toric IOL implantation is to obtain the correct axis and amount of cylinder to be corrected. She usually uses the axis of astigmatism obtained with the Pentacam (Oculus,
Dr. Tyson uses several diagnostic methods to assess both the magnitude and axis of astigmatism preoperatively including autokeratometry, IOLMaster (Carl Zeiss Meditec,
In addition to using the Pentacam to help determine the regularity of the patient's astigmatism, Dr. Tyson uses the preop measurements as a basis for comparison with measurements derived from intraop aberrometry with the VerifEye ORA wavefront intraoperative aberrometry system (WaveTec Vision,
"Ultimately, we base our final determinations on the VerifEye due to its accuracy in determining the steep axis, the power of the toric lens to implant and the proper alignment of the lens on this axis," Dr. Tyson said. "The device can also uniquely take into account the effect of posterior corneal astigmatism, which is difficult to measure preoperatively."
When marking the axis, Dr. Talley Rostov has patients sit upright for initial marking. In the operating room, she uses the intraoperative aberrometer and marks the axis under the microscope. Positioning the patient's head and having the patient looking directly at the microscope light are important to be sure that the toric marks on the IOL align with the toric marks at the limbus.
Dr. Tyson does not mark the steep axis of astigmatism preop or use reference marks on the cornea due to "exceptional" toric lens alignment from intraop aberrometry.
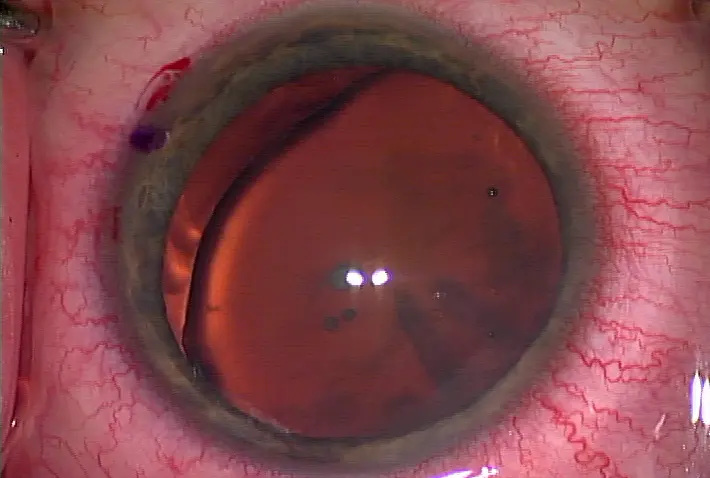
Among the keys to ensuring the toric lens ends up positioned at the planned axis at the end of surgery is a symmetric, well-centered capsulorhexis that encompasses the toric lens edge, Dr. Tyson said. Additionally, he removes all viscoelastic from behind the lens to minimize the opportunity for lens malrotation.
Dr. Talley Rostov agreed about the importance of the intraoperative aberrometer to help with correct placement of the toric IOL at the end of surgery. "I use the VerifEye software of the ORA, and it will tell you in 'real time' whether to rotate the IOL clockwise or counterclockwise for best placement," Dr. Talley Rostov said.
Additional pearls
To ensure optimum toric IOL outcomes with astigmatism, Dr. Talley Rostov aims to account for the natural drift over time toward against-the-rule astigmatism. To offset this effect, she leaves a small amount of with-the-rule astigmatism at the end of the case. "Undercorrect with-the-rule cylinder and overcorrect against-the-rule cylinder so that ideally residual cylinder is less than 0.25 D to 0.50 D with-the-rule," Dr. Talley Rostov said. "The best results are obtained with patients with regular astigmatism."
Additionally, it is important to ensure that any ocular surface disease, such as dry eye, is adequately treated before obtaining measurements and performing cataract surgery.
Dr. Tyson's plan for a mild against-the-rule shift with age leads him to target a postop goal of 0.25 D to 0.50 D of with-the-rule anterior corneal astigmatism, even if he has to flip the axis to achieve that. "Despite all this planning and preparation, one can still have uncontrollable intangibles and end up with residual, off-axis astigmatism," Dr. Tyson said. "Just be prepared to handle these eventualities postoperatively by methods such as lens rotation or exchange, excimer laser ablation or incisional treatment, or glasses or contacts."
Editors' note: Dr. Tyson has financial interests with WaveTec. Dr. Talley Rostov has no financial interests related to this article.
Contact information
Talley Rostov: atalleyrostov@nweyes.com
Tyson: sydtyson@comcast.net


留言
張貼留言