Pseudophakic dysphotopsia Understanding positive dysphotopsia
Pseudophakic dysphotopsia Understanding positive dysphotopsia
by Michelle Dalton EyeWorld Contributing Writer |
The visual disturbances exacerbated by ocular surgery can range from annoying to disabling
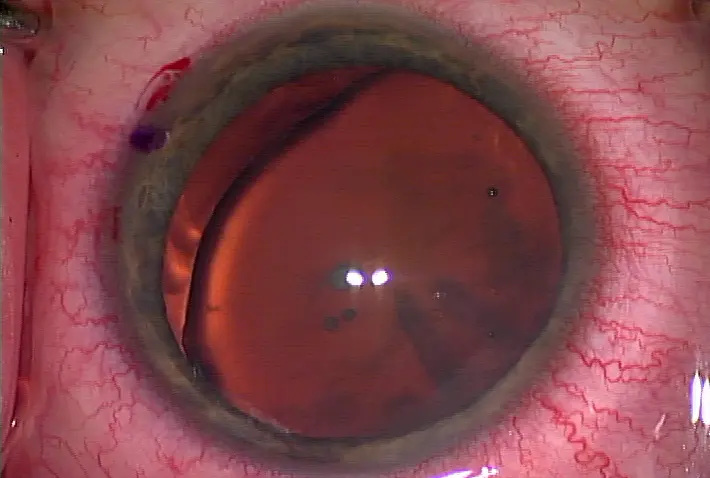
Positive dysphotopsia—the unwanted images including rings, arcs, and central flashes that become bothersome after IOL implantation—have been associated with everything from the patient's ability to recognize the edge of the implanted IOL to corneal disease to multifocal IOLs to an oversized peripheral iridotomy (PI) that allows too much light scatter in the back of the retina. Like most visual anomalies post-surgery, it's nearly impossible to determine who will be affected and who will not beyond a generalized "anyone who is at risk for glare or halo postop."
Numbers may not bear it out, as positive dysphotopsia may not result in an IOL exchange but will result in substantial additional chair time after uneventful cataract surgery. In short, these patients are unhappy, and the wrong approach to take is to reinforce the surgery was "perfect."
Frosting or texturing the edge of the IOL can help reduce—but not eliminate—the occurrence of positive dysphotopsia, Dr. Holladay said.
In Europe, the need to create a PI as part of the Visian ICL (STAAR Surgical, Monrovia, Calif.) procedure has been eliminated by the latest iteration of the implant, but again, that version is not available in the U.S.
In the U.S., square-edged IOLs were developed to try and prevent PCO, but the square-edge design led to patients having portions of their retina exposed to reflected light from the optic edge in addition to refracted light from the central optic, Dr. Kieval said. "The location of the end of the peripheral functional retina is an important factor in negative dysphotopsia. There is no simple way to measure this preoperatively so patients at risk for this phenomenon cannot currently be identified, except it is more likely in the second eye if it occurred in the first," Dr. Holladay said. "Rounded-edge IOLs would reduce the incidence, but it is not worth the increased rate of PCO."
When to treat?
Dr. Kieval believes there are more patients affected by these dysphotopsias than are reported, mainly because it's not typically asked about during the follow-up visits. Also, patients may not mention the dysphotopsia unless their daily lives are being significantly impacted, "which is thankfully not too frequently," he said.
Additional chair time may be necessary to fully grasp the patient's level of discomfort, but in general, if the patient has merely noticed the dysphotopsia but is not complaining about it, "there is no reason for intervention," Dr. Holladay said. "Anterior capsule opacification often ameliorates the symptoms, so intervention is rare."Dr. Kieval also prefers to use IOLs with zero asphericity in patients with irregular corneas "because negative aspheric lenses can potentially contribute to positive dysphotopsia if they're not perfectly centered, and can induce other higher order aberrations because the cornea is, essentially, already aberrated."
Dr. Holladay disagrees, saying "there is no evidence that asphericity has any relationship to dysphotopsias; it is primarily a result of edge design. The improvement of one line of visual acuity, 0.3 log units of contrast sensitivity, and a reduced reaction time with night driving of 0.3 seconds with aspheric IOLs with negative spherical aberration to compensate for the positive corneal spherical aberration has been the single most significant improvement in IOL optical performance in the past 20 years."
How to treat?
"Ideally, you want to get the patient back to emmetropia by eliminating the residual refractive error," he said, and also recommends evaluating the eye to determine if there are any corneal abnormalities such as epithelial basement membrane disease or microstriae in eyes with previous LASIK. If it is a diffractive multifocal IOL, surgeons must ensure that the IOL is not tilted and is centered to slightly nasal in the pupil, "as it must not be decentered temporally," Dr. Holladay said.
"Patients who need intervention have to be handled on a case-by-case basis and their complaint is usually of 'waxy vision,'" he said. With both positive and negative dysphotopsia, Nd:YAG removal of the nasal capsule overlying the IOL may be helpful, and secondary piggyback silicone IOLs with rounded edges in most cases will eliminate the symptoms. As peripheral capsular opacification may eliminate the problem, it is prudent to wait a few months to be sure the problem does not disappear by itself, Dr. Holladay said.
Dr. Kieval will not intervene early on if it is related to the IOL, but rather wait for a few months and try to postpone treatment.
"If we can rule out causes other than the IOL design, I explain that most of the aberrations resolve with time," he said.
For patients who cannot adapt after 3 to 6 months postop, Dr. Kieval will perform an IOL exchange.
"We work with the patients throughout that time frame to ensure they're comfortable with the decision to wait and see," he said. "This can be especially crucial in multifocal patients." For multifocal patients, that means a lens exchange to either a monofocal or accommodating, in order to eliminate the multifocal rings altogether. "Choosing a lens with a round optic edge or a silicone lens is a good option when exchanging the IOL in these patients," he said. What surgeons need to remember about the phenomenon is that likely about 20% of people with a square-edge optic IOL will experience some kind of positive dysphotopsia, but of those 20%, only around 10% will say it's noticeable or bothersome, Dr. Kieval said.References
Holladay JT, Lang A, Portney V. Analysis of edge glare phenomena in intraocular lens edge designs. J Cataract Refract Surg 1999; 25:748–52.
Holladay JT, Zhao H, Reisin CR. Negative dysphotopsia: The enigmatic penumbra. J Cataract Refract Surg. 2012 Jul; 38(7): 1251–65.
Editors' note: Dr. Holladay has financial interests with Alcon (Fort Worth, Texas). Dr. Kieval has financial interests with Abbott Medical Optics (Santa Ana, Calif.) and Lenstec (St. Petersburg, Fla.). Dr. Trattler has financial interests with Abbott Medical Optics and Bausch + Lomb (Rochester, N.Y.).


留言
張貼留言