Challenging refractive cases Dodgy DLK diagnosis
August 2010‧EyeWorld
Challenging refractive cases Dodgy DLK diagnosis
by Maxine Lipner Senior EyeWorld Contributing Editor
Eye with diffuse interface fluid syndrome Source: Richard L. Lindstrom, M.D.
It must have seemed like an easy diagnosis, a no-brainer even. Following bilateral LASIK for high myopia, a 31-year-old man returned a few days later complaining of blurry vision with his eyes showing mild irritation. Initially the patient had acuity of 20/30 in both eyes, with an intraocular pressure of 18mmHg. The surgeon here concluded that this was yet another case of DLK and treated the patient with intense steroids, placing him initially on 1 percent prednisolone acetate to be taken every two hours. At the 3-week post-op mark, however, no improvement was seen in the DLK appearance. The patient's vision was not checked, but his pressure had climbed to 23 mmHg in both eyes. His physician once again labeled this as persistent DLK and increased the frequency of the administration of the 1% prednisolone acetate to once every hour in both eyes. In addition, the patient was placed on oral prednisone, as well as Alphagan P (brimonidine tartrate, Allergan, Irvine, Calif.) and 0.5% Timolol, both to be taken twice a day. By the time the patient's vision was checked at week 4 it was 20/60 in the right eye and 20/200 in the left. The surgeon here continued to treat this as persistent DLK. The flap of the left eye was lifted and irrigated and the patient was continued on his medication. When the patient returned for his 5 week visit his vision was "still blurry." At this point his acuity was less than 20/400 in both eyes. When a hard contact was placed over his right eye his acuity improved to 20/60, however, when this was tried with the left eye no improvement was seen. At this point the patient was continued on medication and finally referred to Richard L. Lindstrom, M.D., adjunct professor emeritus, Department of Ophthalmology, University of Minnesota, Minneapolis, and founder, Minnesota Eye Consultants, Minneapolis.
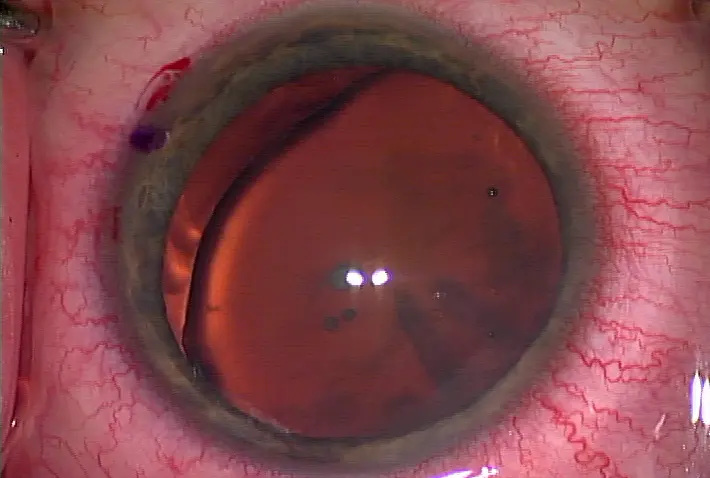
DLK Source: Elizabeth A. Davis, M.D.
The wrong diagnosis
By the time he arrived for the post-op consultation with Dr. Lindstrom at 7 weeks, the patient was totally disabled and unable to walk without assistance. His vision in his right eye was 20/100 and in his left had diminished to light perception only. When Dr. Lindstrom examined the patient at the slitlamp he saw epithelial micro cystic edema in the periphery of the eye and an optically clear fluid-filled interface. The patient's intraocular pressure as measured by applanation tonometry was 0 mmHg in the right eye and 1 mmHg in the left. However, when the Tono-pen was used in the periphery the pressure was 30 mmHg in the right eye and 40 mmHg in the left. Damage to the visual fields was seen with superior and inferior thinning of the cup margin.
Dr. Lindstrom realized that a mistake had been made here—the patient never had DLK. Instead Dr. Lindstrom diagnosed him with diffuse interface fluid syndrome, a condition that can sometimes simulate DLK. "The patient was a steroid-responder and developed glaucoma—he did not actually have DLK," Dr. Lindstrom said. "What happens is that fluid actually collects in the space between the flap and the cornea and that is such that when you check the pressure it actually measures soft even though it's really high." In effect what is being measured in an artificial anterior chamber that has been created between the flap and the cornea, rather than the actual pressure inside of the eye. The correct diagnosis of diffuse interface fluid syndrome was missed here. "There is a sort of classic slitlamp appearance," Dr. Lindstrom said. "In addition, if you're measuring a softer than normal pressure it's something that you should look for." Dr. Lindstrom stopped the steroids, but continued the patient on the Alphagan P and Timolol twice a day. He also added Xalatan (latanoprost, Pfizer, New York) and Diamox (acetazolamide, Wyeth-Ayerst Laboratories, Collegeville, Pa.) to the mix. "I stopped the steroids, put the patient on anti-hypertensive's and everything healed up," Dr. Lindstrom said. "But the patient had significant glaucoma damage." At the 8-week postoperative mark the patient's vision in the right eye was 20/40 and 20/50 in the left eye. The pressure in both eyes was down to 10 mmHg. At the slitlamp Dr. Lindstrom saw that the microcystic and interface edema was resolving. Unfortunately, the fundus exam showed vertical cup enlargement with superior and inferior thinning of the cup margin. The damage to the field had unfortunately been done.
Dr. Lindstrom sees this as the sort of case that others can learn from. "The most common complication today after LASIK is DLK and the treatment is steroids," he said. "But with the typical DLK you should see the patient back in two to three days, and if they're not better you lift the flap and irrigate out the interface and then it usually responds." He points out that typical DLK does not last more than a week to 10 days without responding or becoming worse. "They pretty much all respond if they're treated," Dr. Lindstrom said. "So, if you've got a patient out a couple of weeks and you're looking at the cornea and it doesn't look right it's not DLK." Dr. Lindstrom stresses that the treatment isn't just more and more steroids particularly in myopes. "The typical myope is more vulnerable to optic nerve damage and when you're using long-term full strength steroids like prednisone acetate or today Durasal and even in this case systemic steroids, you have to be nervous that this patient could be a steroid responder and develop glaucoma."
Looking for diffuse interface fluid syndrome
Diffuse interface fluid syndrome should have been on the physician's radar. Hallmarks of the condition can initially appear similar to DLK. "From the patient's perspective they have blurry vision, which would be consistent with DLK as well," Dr. Lindstrom said. "They have blurry vision and they don't have a red, inflamed eye." In addition Dr. Lindstrom finds that the cornea is often mildly edematous which can also be consistent with DLK. However, this is where the conditions diverge. "When you look in the interface with DLK you see white blood cells and you see a tight interface with white blood cells in the interface," Dr. Lindstrom said. "Then most people stage it 1, 2, 3, 4, depending if there are a few diffuse cells in the periphery, if they spread all the way across the interface, if they are starting to clump, or in stage 4 if you see some melting and damage."
Diffuse interface syndrome, however, appears differently. "With diffuse interface syndrome you actually see a fluid cleft in the interface rather than white blood cells," Dr. Lindstrom said. "Then when you measure the pressure you measure a really low pressure like two to four centrally but if you were to take an applanation tonometer or a pneumotonometer and measure the pressure outside the flap you would measure 30 or 40 or 57.’’
If a practitioner is aware of the condition it's usually easy to detect. "You can make the diagnosis just looking for it," Dr. Lindstrom said. Then the treatment is the exact opposite of that for DLK. "The treatment in DLK is intense steroids," Dr. Lindstrom said. "The treatment in diffuse interface fluid syndrome is to stop all the steroids and treat with antihypertensive to lower the pressure."
Usually determining whether a case is ordinary DLK or diffuse interface fluid syndrome comes down to a differential diagnosis. Dr. Lindstrom finds that DLK usually starts with just a few cells on the first day and gets worse by day 3. "If you lift the flap and irrigate then it is usually better within 1 week with a short-term course of intense steroids," he said. "But if you've got something that is more than one week out then it is probably not the acute problem of DLK." It then comes down to making the differential diagnosis and considering what else can cause corneal edema and reduce vision. "One of those things is this diffuse interface fluid syndrome, another one could be an infection," Dr. Lindstrom said. "But then you'd see infiltrate, you'd have a red eye, and there might be a hypopyon." Another possibility to consider might be corneal endothelial cell failure for example in a Fuch's dystrophy patient. However, Dr. Lindstrom points out that this is unlikely. "You usually wouldn't have done surgery on such a patient," he said. "So, the differential really comes down to DLK versus this diffuse interface fluid syndrome and if you have never seen one, don't know what it looks like, don't have it in mind you can miss it and just keep piling on the steroids—that's what happened in this case."
In the end, the patient paid the price here. "The patient's vision came back but he had significant field loss," Dr. Lindstrom said. "If a diagnosis had been made promptly and the pressure was just elevated for a few days, there would not have been any damage—it's the extended elevation that was missed."
Editors' note: Dr. Lindstrom has no financial interests related to his comments.
Contact information
Lindstrom: 612-813-3633, rllindstrom@mneye.com






留言
張貼留言