Diagnosing dry eye
Diagnosing dry eye
by Michelle Dalton EyeWorld Contributing Editor
Clinical signs and patient-reported symptoms may not correlate; patient symptoms must take precedence

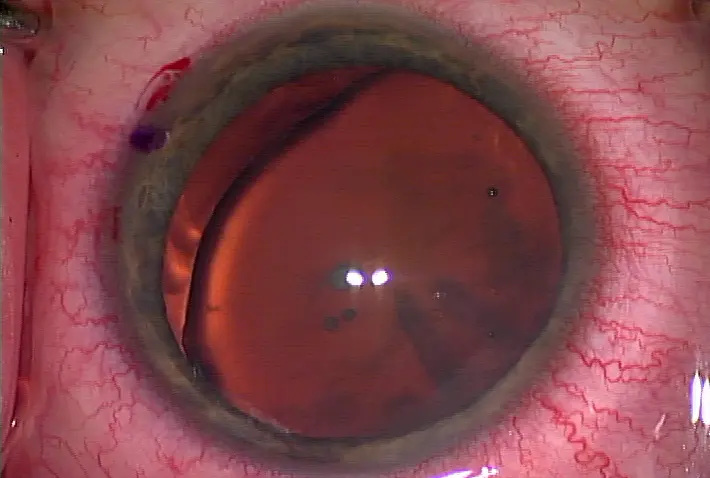
An eye with a poor tear film surface Source: Gary Foulks, M.D.

Lissamine green staining helps clarify the severity of the ocular surface

Poor tear break-up time is also indicative of increased dry eye severity Source: Gary Foulks, M.D.
One of the most common reasons people visit eyecare specialists is due to complaints of dry eye, yet specialists and those in general practice believe the numbers are wildly underestimated. "In my practice, 40-50% will have some form or complaint of ocular surface dysfunction," said Christopher E. Starr, M.D., assistant professor of ophthalmology, and director, cornea, cataract, and refractive surgery fellowship and service, Weill Cornell Medical College, New York. According to Caroline Blackie, O.D., Ph.D., clinical research scientist, Korb Associates, Boston, and TearScience, Morrisville, N.C., in the winter months (January-March) "somewhere between 35% and 40% of patients have some complaint related to dryness in our general practice. In the summer months, it's somewhat less—maybe closer to 20-25% of people who come in without referrals."
While the incidence of dry eye might fluctuate depending on geography, "there's an understanding of what constitutes dry eye that's beginning to change as well," said Michael A. Lemp, M.D., clinical professor of ophthalmology, Georgetown University, and George Washington University, Washington, D.C., and chief medical officer, TearLab, San Diego. As defined by the Dry Eye Workshop Study Group (DEWS) in 2007, dry eye is a multifactorial disease of the ocular surface that includes an element of inflammation; it is also accompanied by increased osmolarity. Perhaps as a result of the DEWS report, clinicians are now more aware of dry eye and are actively looking to treat it. Not only is the percentage of patients who present with primary complaints of dry eye much higher than some estimates suggest, "there is a group of patients who come in for some other complaint but have significant ocular surface disease as a secondary diagnosis," said Edward J. Holland, M.D., professor of ophthalmology, University of Cincinnati, and director of cornea, Cincinnati Eye Institute. For instance, Dr. Holland said, when analyzing his cataract population, the incidence of meibomian gland dysfunction (MGD) with evaporative dry eye is "very high. So when people complain of decreased vision and you're thinking about cataract surgery, you may inadvertently overlook an important secondary diagnosis of MGD. Although that's not what the patient came in for, it will affect the surgical outcomes of anterior segment surgery."
The number of people who come into a practice without thinking they have any dry eye component "is very high as well. But a significant number of those people will have some kind of dry eye," said Donald R. Korb, O.D., founder, Korb Associates, and co-founder, TearScience.
Compounding the issue is the fact that lid margin disease is "officially considered dry eye, but the problem is primarily lid margin disease with evaporative dry eye," said Gary Foulks, M.D., emeritus professor of ophthalmology, department of ophthalmology and visual sciences, University of Louisville School of Medicine, Ky.
When people do present with dry eye, "mild dry eye can have severe symptoms, and people with severe dry eye can report no symptoms," Dr. Starr said. Chronic severe dry eye can cause damage to the corneal nerves; "the nerves become relatively desensitized with a reduction in corneal sensation—hence less pain and fewer complaints—but the surface looks like a complete mess at the slit lamp." An individual's pain tolerance will also factor into the magnitude of complaints, Dr. Starr added. "There are patients with 20/70 vision who have no complaints or reduction in daily functioning, and then there are those with 20/25 vision who are miserable; similarly, the discordance between dry eye signs and symptoms in some patients is related to an individual's tolerance level and personality," he said.
Lifestyle choices
A decade ago, clinicians expected those in the computer field to have increased levels of dry eye compared to their counterparts, Dr. Blackie said, with a "marked difference" between software engineers and others. With the influx of computer games, smartphones, and online gaming, however, "there's an expanding age range. As few as 15 years ago, we rarely heard of children with dry eye complaints. For risk factors, lifestyle is a tremendously important factor; age and gender are not as definitive as they used to be," she said.
People who predominantly use computers for hours at a time have reduced blink rates, which will exacerbate any ongoing dry eye complaints, Dr. Starr said. "When you're working on a computer, your blink rate decreases, sometimes by 50%, leading to increased tear evaporation, surface dryness, and all the typical symptoms of dysfunctional tear syndrome," he said. Add forced air systems to the mix, and computer vision syndrome becomes even worse, leading to dryness, accommodative fatigue, and headaches, Dr. Starr said. "The pervasive presence of the computer in our daily lives is the culprit for numerous complaints," he said. "Patients who are otherwise healthy present with increased evaporative dry eye because of the decreased blink rate and high inter- blink fluctuations throughout the day. Often when these same people go home and relax, the blink rate returns to normal and the symptoms dissipate." These kinds of "transient" dry eye patients may be managed with artificial tears and simple lifestyle modifications, he said.
Diagnostic dilemmas
As recently as a decade ago, "everyone thought dry eye was solely aqueous deficiency and we treated it with artificial tears," Dr. Foulks said. Now clinicians are aware of MGD and evaporative dry eye, and "most cases are a hybrid type of dry eye that's both aqueous deficient with MGD and/or evaporative," he said. Chronic dry eye patients can be frustrating, and diagnosis of the correct ocular surface disease can sometimes be challenging, Dr. Holland said. "However, we have a much bigger problem on the treatment side than on the diagnostic side."
Dr. Korb said if clinicians were to conduct "a complete dry eye evaluation using the entire spectrum of tests, three separate visits would be required to differentiate what the underlying causes of the complaint might be." What is the one best "test" for diagnosing most patients? A careful and detailed patient history, he said.
Clinicians need to think about "the main causes of ocular surface disease overall," Dr. Holland said. "Listen to the patient. We're trying to differentiate between aqueous tear deficiency, anterior blepharitis, MGD that leads to evaporative dry eye, and ocular allergies. Those are the four big ocular surface diseases. The problem for clinicians is that symptoms may overlap among the diseases. Complaints of irritation, burning, and redness are common to all these diagnoses. We have to pay attention to the clues."
One reason patient symptoms are so valuable is because "we don't have one test that's going to tell us this is dry eye and it's because of one mechanism or a bunch of mechanisms," Dr. Foulks said. As clinicians learn more about dry eye, a quick slit lamp exam of only the cornea is no longer enough, Dr. Holland said. "We need to carefully evaluate the lid function and tear film. We need conjunctival and corneal epithelium evaluations. We need to use vital dyes and fluorescein staining. Another important diagnostic tool that we often forget is to take a careful history and have a discussion about symptoms with the patient," he said. Dr. Blackie also opts for "history and symptomatology first." Because physicians have limited time with the patient—10-20 minutes in the chair at most, she said—"never toss out symptoms because some of the clinical signs may not match. That doesn't mean to pick one over the other—always consider both signs and symptoms." Identifying those with severe disease is often much easier than identifying those in earlier stages, Dr. Lemp said. For instance, Schirmer's test scores are likely normal in people in the early to moderate stages; the test measures lacrimal damage, not meibomian gland damage, so it will not assess evaporative dry eye accurately, he said.
"The bottom line—be a doctor. Listen to the patient. You cannot take the patient out of this diagnostic equation," he said.
If patients have "severe surface disease but are not complaining, that indicates chronicity and puts them into a much more severe category. They've lost corneal sensation and don't appreciate the dysfunction of the tear any longer," Dr. Foulks said. The type of dry eye will dictate whether Dr. Foulks first recommends an artificial tear with a lipid component (for predominantly evaporative dry eye) or a tear that increases the volume alone or that protects against elevated osmolarity. There remains a "huge need for objective measurement with an unbiased measure of tear film quality and status," Dr. Starr said. "We've known for years that increased tear osmolarity is an important diagnostic finding," but it was too cumbersome in the past to evaluate. A new diagnostic tool, the TearLab osmolarity test, "is probably the most reliable measure of determining if there is dry eye, but you need at least one additional test to determine what kind of dry eye," Dr. Foulks said.
"In terms of patient acceptance, they like the osmolarity test because it's less invasive and gives them a number they can wrap their mind around. Osmolarity has a baseline of 308—above that and you've got dry eye, below that and you don't," Dr. Lemp said. For Dr. Foulks, osmolarity is also a measure to ensure the treatment regimen is working. "When patients report they feel better, osmolarity can confirm their eyes are improving clinically, as the number goes down as well. If I have a patient who doesn't notice a lot of improvement but the osmolarity is decreasing, then I know there's evidence we're on the right treatment track."
Summarized Dr. Lemp: The tear film osmolarity test "parallels disease severity. Osmolarity is still variable, but it's the least variable of any of the tests we currently have."
Another potential diagnostic test is the InflammaDry (Rapid Pathogen Screening, Sarasota, Fla.), which detects the matrix metalloproteinase 9 (MMP-9) protein. Increased levels of MMP-9 have been previously reported in the tear fluid of those with dry eye. TearLab also has a platform that may potentially be able to measure lactoferrin, but does not yet have a test, Dr. Foulks said. According to Dr. Holland, the TearScience LipiFlow "is positioned around the lower lid and heats up the meibomian glands to a specific temperature. In clinical trials it showed a better function of the meibomian glands and better flow of meibum, in turn creating a better quality tear film." The device is still under investigation in the U.S., he added.
Evaluating the unknown
One problem for those investigating dry eye is "we don't know what we don't know," Dr. Korb said. For instance, until recently the role of the eyelid and lid wiper in dry eye was unknown, but now about 80% of those with dry eye also have some level of lid wiper epitheliopathy, said Drs. Korb and Blackie. Although inflammation is now a given for those with dry eye, researchers have not yet been able to sufficiently identify all the inflammatory cytokines in tears, Dr. Lemp said. Conversely, a drug such as topical azithromycin (AzaSite, Inspire Pharmaceuticals, Durham, N.C.) has shown great promise in treating MGD, "but we're still waiting for FDA approval for that indication," Dr. Holland said. "It's a frustrating relationship ophthalmologists have with the FDA; we're still trying to figure out the right test that can show how this drug is effective."
Dr. Starr agreed, noting that MGD and blocked glands are major players in dry eye. "Just treating the lids won't be enough. I recommend azithromycin off label for blepharitis for 2-4 weeks." In fact, "any component of lid disease" should be prescribed azithromycin, but not as a standalone treatment until clinicians have more information. "The MGD Workshop findings are going to do for MGD what the DEWS report did for dry eye and will lead us to (hopefully) realize even more about what we don't know yet," he said.
A relatively unexamined area "is inflammation we cannot see with the slit lamp," Dr. Blackie added. "Non-obvious inflammation needs tools we don't necessarily have available to diagnose." For instance, confocal microscopy may help identify areas of inflammation in the lids and cornea not visible with the slit lamp, she suggested. In short, "we need better tests and better tools," she said.
Non-obvious MGD "explains why so many people under 40 have dry eye," Dr. Korb said. "We're making progress in correlating the signs and symptoms, but we are not quite there yet."
Dry eye and ocular surgery
A diagnosis of dry eye need not prevent someone from undergoing ocular surgery, but surgeons should be aware that the state of the ocular surface will dictate those "who are likely to have tear instability problems after the stress of surgery or who might have more complaints about visual outcomes," Dr. Foulks said. In moderate-to-severe dry eye, patients are more likely to have complications post-op, he added. "The threshold for performing surgery on someone with dry eye needs to be higher," he said.
The key, Dr. Starr said, is to stabilize the ocular surface before taking any pre-op measurements for premium IOLs or laser vision correction. "If you get patients to a point where they have an optimized and stable ocular surface, not only before doing the surgery but before taking your final pre-op measurements, your outcomes will be much better and your patients will be happier," he said.
Editors' note: Dr. Blackie has a financial interest with TearScience. Dr. Foulks has financial interests with Alcon (Fort Worth, Texas), Acucela (Seattle), Bausch & Lomb (Rochester, N.Y.), Inspire Pharmaceuticals, InSite Vision (Alameda, Calif.), Merck (Whitehouse Station, N.J.), Pfizer (New York), Santen (Napa, Calif.), and TearLab. Dr. Holland has financial interests with Bausch & Lomb and Inspire Pharmaceuticals. Dr. Korb has financial interests with Alcon and Ocular Research of Boston. Dr. Lemp has financial interests with numerous companies investigating dry eye treatments. Dr. Starr has financial interests with Allergan (Irvine, Calif.) and Inspire Pharmaceuticals.
Contact information
Blackie: 781-229-2020, CBlackie@tearscience.com
Foulks: 502-852-6150, gnfoul01@louisville.edu
Holland: 859-331-9000, eholland@holprovision.com
Korb: 617-426-0370, drkorb@aol.com
Lemp: 202-255-6842, malemp@lempdc.com
Starr: 646-962-3370, cestarr@med.cornell.edu
by Michelle Dalton EyeWorld Contributing Editor
Clinical signs and patient-reported symptoms may not correlate; patient symptoms must take precedence
An eye with a poor tear film surface Source: Gary Foulks, M.D.
Lissamine green staining helps clarify the severity of the ocular surface
Poor tear break-up time is also indicative of increased dry eye severity Source: Gary Foulks, M.D.
One of the most common reasons people visit eyecare specialists is due to complaints of dry eye, yet specialists and those in general practice believe the numbers are wildly underestimated. "In my practice, 40-50% will have some form or complaint of ocular surface dysfunction," said Christopher E. Starr, M.D., assistant professor of ophthalmology, and director, cornea, cataract, and refractive surgery fellowship and service, Weill Cornell Medical College, New York. According to Caroline Blackie, O.D., Ph.D., clinical research scientist, Korb Associates, Boston, and TearScience, Morrisville, N.C., in the winter months (January-March) "somewhere between 35% and 40% of patients have some complaint related to dryness in our general practice. In the summer months, it's somewhat less—maybe closer to 20-25% of people who come in without referrals."
While the incidence of dry eye might fluctuate depending on geography, "there's an understanding of what constitutes dry eye that's beginning to change as well," said Michael A. Lemp, M.D., clinical professor of ophthalmology, Georgetown University, and George Washington University, Washington, D.C., and chief medical officer, TearLab, San Diego. As defined by the Dry Eye Workshop Study Group (DEWS) in 2007, dry eye is a multifactorial disease of the ocular surface that includes an element of inflammation; it is also accompanied by increased osmolarity. Perhaps as a result of the DEWS report, clinicians are now more aware of dry eye and are actively looking to treat it. Not only is the percentage of patients who present with primary complaints of dry eye much higher than some estimates suggest, "there is a group of patients who come in for some other complaint but have significant ocular surface disease as a secondary diagnosis," said Edward J. Holland, M.D., professor of ophthalmology, University of Cincinnati, and director of cornea, Cincinnati Eye Institute. For instance, Dr. Holland said, when analyzing his cataract population, the incidence of meibomian gland dysfunction (MGD) with evaporative dry eye is "very high. So when people complain of decreased vision and you're thinking about cataract surgery, you may inadvertently overlook an important secondary diagnosis of MGD. Although that's not what the patient came in for, it will affect the surgical outcomes of anterior segment surgery."
The number of people who come into a practice without thinking they have any dry eye component "is very high as well. But a significant number of those people will have some kind of dry eye," said Donald R. Korb, O.D., founder, Korb Associates, and co-founder, TearScience.
Compounding the issue is the fact that lid margin disease is "officially considered dry eye, but the problem is primarily lid margin disease with evaporative dry eye," said Gary Foulks, M.D., emeritus professor of ophthalmology, department of ophthalmology and visual sciences, University of Louisville School of Medicine, Ky.
When people do present with dry eye, "mild dry eye can have severe symptoms, and people with severe dry eye can report no symptoms," Dr. Starr said. Chronic severe dry eye can cause damage to the corneal nerves; "the nerves become relatively desensitized with a reduction in corneal sensation—hence less pain and fewer complaints—but the surface looks like a complete mess at the slit lamp." An individual's pain tolerance will also factor into the magnitude of complaints, Dr. Starr added. "There are patients with 20/70 vision who have no complaints or reduction in daily functioning, and then there are those with 20/25 vision who are miserable; similarly, the discordance between dry eye signs and symptoms in some patients is related to an individual's tolerance level and personality," he said.
Lifestyle choices
A decade ago, clinicians expected those in the computer field to have increased levels of dry eye compared to their counterparts, Dr. Blackie said, with a "marked difference" between software engineers and others. With the influx of computer games, smartphones, and online gaming, however, "there's an expanding age range. As few as 15 years ago, we rarely heard of children with dry eye complaints. For risk factors, lifestyle is a tremendously important factor; age and gender are not as definitive as they used to be," she said.
People who predominantly use computers for hours at a time have reduced blink rates, which will exacerbate any ongoing dry eye complaints, Dr. Starr said. "When you're working on a computer, your blink rate decreases, sometimes by 50%, leading to increased tear evaporation, surface dryness, and all the typical symptoms of dysfunctional tear syndrome," he said. Add forced air systems to the mix, and computer vision syndrome becomes even worse, leading to dryness, accommodative fatigue, and headaches, Dr. Starr said. "The pervasive presence of the computer in our daily lives is the culprit for numerous complaints," he said. "Patients who are otherwise healthy present with increased evaporative dry eye because of the decreased blink rate and high inter- blink fluctuations throughout the day. Often when these same people go home and relax, the blink rate returns to normal and the symptoms dissipate." These kinds of "transient" dry eye patients may be managed with artificial tears and simple lifestyle modifications, he said.
Diagnostic dilemmas
As recently as a decade ago, "everyone thought dry eye was solely aqueous deficiency and we treated it with artificial tears," Dr. Foulks said. Now clinicians are aware of MGD and evaporative dry eye, and "most cases are a hybrid type of dry eye that's both aqueous deficient with MGD and/or evaporative," he said. Chronic dry eye patients can be frustrating, and diagnosis of the correct ocular surface disease can sometimes be challenging, Dr. Holland said. "However, we have a much bigger problem on the treatment side than on the diagnostic side."
Dr. Korb said if clinicians were to conduct "a complete dry eye evaluation using the entire spectrum of tests, three separate visits would be required to differentiate what the underlying causes of the complaint might be." What is the one best "test" for diagnosing most patients? A careful and detailed patient history, he said.
Clinicians need to think about "the main causes of ocular surface disease overall," Dr. Holland said. "Listen to the patient. We're trying to differentiate between aqueous tear deficiency, anterior blepharitis, MGD that leads to evaporative dry eye, and ocular allergies. Those are the four big ocular surface diseases. The problem for clinicians is that symptoms may overlap among the diseases. Complaints of irritation, burning, and redness are common to all these diagnoses. We have to pay attention to the clues."
One reason patient symptoms are so valuable is because "we don't have one test that's going to tell us this is dry eye and it's because of one mechanism or a bunch of mechanisms," Dr. Foulks said. As clinicians learn more about dry eye, a quick slit lamp exam of only the cornea is no longer enough, Dr. Holland said. "We need to carefully evaluate the lid function and tear film. We need conjunctival and corneal epithelium evaluations. We need to use vital dyes and fluorescein staining. Another important diagnostic tool that we often forget is to take a careful history and have a discussion about symptoms with the patient," he said. Dr. Blackie also opts for "history and symptomatology first." Because physicians have limited time with the patient—10-20 minutes in the chair at most, she said—"never toss out symptoms because some of the clinical signs may not match. That doesn't mean to pick one over the other—always consider both signs and symptoms." Identifying those with severe disease is often much easier than identifying those in earlier stages, Dr. Lemp said. For instance, Schirmer's test scores are likely normal in people in the early to moderate stages; the test measures lacrimal damage, not meibomian gland damage, so it will not assess evaporative dry eye accurately, he said.
"The bottom line—be a doctor. Listen to the patient. You cannot take the patient out of this diagnostic equation," he said.
If patients have "severe surface disease but are not complaining, that indicates chronicity and puts them into a much more severe category. They've lost corneal sensation and don't appreciate the dysfunction of the tear any longer," Dr. Foulks said. The type of dry eye will dictate whether Dr. Foulks first recommends an artificial tear with a lipid component (for predominantly evaporative dry eye) or a tear that increases the volume alone or that protects against elevated osmolarity. There remains a "huge need for objective measurement with an unbiased measure of tear film quality and status," Dr. Starr said. "We've known for years that increased tear osmolarity is an important diagnostic finding," but it was too cumbersome in the past to evaluate. A new diagnostic tool, the TearLab osmolarity test, "is probably the most reliable measure of determining if there is dry eye, but you need at least one additional test to determine what kind of dry eye," Dr. Foulks said.
"In terms of patient acceptance, they like the osmolarity test because it's less invasive and gives them a number they can wrap their mind around. Osmolarity has a baseline of 308—above that and you've got dry eye, below that and you don't," Dr. Lemp said. For Dr. Foulks, osmolarity is also a measure to ensure the treatment regimen is working. "When patients report they feel better, osmolarity can confirm their eyes are improving clinically, as the number goes down as well. If I have a patient who doesn't notice a lot of improvement but the osmolarity is decreasing, then I know there's evidence we're on the right treatment track."
Summarized Dr. Lemp: The tear film osmolarity test "parallels disease severity. Osmolarity is still variable, but it's the least variable of any of the tests we currently have."
Another potential diagnostic test is the InflammaDry (Rapid Pathogen Screening, Sarasota, Fla.), which detects the matrix metalloproteinase 9 (MMP-9) protein. Increased levels of MMP-9 have been previously reported in the tear fluid of those with dry eye. TearLab also has a platform that may potentially be able to measure lactoferrin, but does not yet have a test, Dr. Foulks said. According to Dr. Holland, the TearScience LipiFlow "is positioned around the lower lid and heats up the meibomian glands to a specific temperature. In clinical trials it showed a better function of the meibomian glands and better flow of meibum, in turn creating a better quality tear film." The device is still under investigation in the U.S., he added.
Evaluating the unknown
One problem for those investigating dry eye is "we don't know what we don't know," Dr. Korb said. For instance, until recently the role of the eyelid and lid wiper in dry eye was unknown, but now about 80% of those with dry eye also have some level of lid wiper epitheliopathy, said Drs. Korb and Blackie. Although inflammation is now a given for those with dry eye, researchers have not yet been able to sufficiently identify all the inflammatory cytokines in tears, Dr. Lemp said. Conversely, a drug such as topical azithromycin (AzaSite, Inspire Pharmaceuticals, Durham, N.C.) has shown great promise in treating MGD, "but we're still waiting for FDA approval for that indication," Dr. Holland said. "It's a frustrating relationship ophthalmologists have with the FDA; we're still trying to figure out the right test that can show how this drug is effective."
Dr. Starr agreed, noting that MGD and blocked glands are major players in dry eye. "Just treating the lids won't be enough. I recommend azithromycin off label for blepharitis for 2-4 weeks." In fact, "any component of lid disease" should be prescribed azithromycin, but not as a standalone treatment until clinicians have more information. "The MGD Workshop findings are going to do for MGD what the DEWS report did for dry eye and will lead us to (hopefully) realize even more about what we don't know yet," he said.
A relatively unexamined area "is inflammation we cannot see with the slit lamp," Dr. Blackie added. "Non-obvious inflammation needs tools we don't necessarily have available to diagnose." For instance, confocal microscopy may help identify areas of inflammation in the lids and cornea not visible with the slit lamp, she suggested. In short, "we need better tests and better tools," she said.
Non-obvious MGD "explains why so many people under 40 have dry eye," Dr. Korb said. "We're making progress in correlating the signs and symptoms, but we are not quite there yet."
Dry eye and ocular surgery
A diagnosis of dry eye need not prevent someone from undergoing ocular surgery, but surgeons should be aware that the state of the ocular surface will dictate those "who are likely to have tear instability problems after the stress of surgery or who might have more complaints about visual outcomes," Dr. Foulks said. In moderate-to-severe dry eye, patients are more likely to have complications post-op, he added. "The threshold for performing surgery on someone with dry eye needs to be higher," he said.
The key, Dr. Starr said, is to stabilize the ocular surface before taking any pre-op measurements for premium IOLs or laser vision correction. "If you get patients to a point where they have an optimized and stable ocular surface, not only before doing the surgery but before taking your final pre-op measurements, your outcomes will be much better and your patients will be happier," he said.
Editors' note: Dr. Blackie has a financial interest with TearScience. Dr. Foulks has financial interests with Alcon (Fort Worth, Texas), Acucela (Seattle), Bausch & Lomb (Rochester, N.Y.), Inspire Pharmaceuticals, InSite Vision (Alameda, Calif.), Merck (Whitehouse Station, N.J.), Pfizer (New York), Santen (Napa, Calif.), and TearLab. Dr. Holland has financial interests with Bausch & Lomb and Inspire Pharmaceuticals. Dr. Korb has financial interests with Alcon and Ocular Research of Boston. Dr. Lemp has financial interests with numerous companies investigating dry eye treatments. Dr. Starr has financial interests with Allergan (Irvine, Calif.) and Inspire Pharmaceuticals.
Contact information
Blackie: 781-229-2020, CBlackie@tearscience.com
Foulks: 502-852-6150, gnfoul01@louisville.edu
Holland: 859-331-9000, eholland@holprovision.com
Korb: 617-426-0370, drkorb@aol.com
Lemp: 202-255-6842, malemp@lempdc.com
Starr: 646-962-3370, cestarr@med.cornell.edu


留言
張貼留言