Taking control of PCO
Taking control of PCO
EyeWorld.APRIL 2011
---------------------------------------------------------
by Marie-Jose Tassignon, M.D., Ph.D.
Although a YAG laser capsulotomy is a simple and quick means of addressing the degradation of visual acuity from posterior capsule opacification, it has potential drawbacks including a small risk of eliciting a retinal detachment and the creation of permanent vitreous floaters. Ideally, the best way of treating posterior capsule opacification is to prevent its development. In this month's column, Marie-Jose Tassignon, M.D., Ph.D., of Belgium, discusses her bag-in-the-lens technique for eradicating posterior capsule opacification. The technique requires more accurate precision in anterior and posterior capsulorhexis creation, but when performed successfully, completely eliminates the need for YAG capsulotomies. The introduction of the femtosecond laser for precise capsulorhexis sizing and placement in combination with Dr. Tassignon's technique may offer surgeons a simplified method of instituting her procedure in the future. Until those devices become available, we will have to rely on our skills and her pearls for performing the bag-in-the-lens method. I believe you will find her discussion stimulating and enlightening.
Richard Hoffman, M.D. Column Editor
Marie-Jose Tassignon, M.D., Ph.D., Antwerp University Hospital, Antwerp, Belgium, discusses the bag-in-the-lens technique
.
The bag-in-the-lens (BIL) procedure is a new concept born out of my desire to design a technique where posterior capsular opacification (PCO) is eradicated. Secondary posterior opacification of the capsular bag incurs a very high social security cost in European countries, including Belgium, where the total population is 10 million and the cost of PCO is approximately 9 million Euros per year for a complication that can be avoided.
The BIL technique consists of implanting a lens that is round. The 5-mm optic is surrounded by a peripheral groove with elliptical haptics. The haptics are perpendicular to one another, allowing for accommodation of both the anterior and posterior capsulorhexis. That means a very precise-sized anterior and posterior capsulorhexis is needed. For this purpose, I developed a capsulorhexis caliper that can easily be inserted through a 1.2-mm opening of a corneal incision. This instrument can certainly be used for all kinds of IOLs as well.
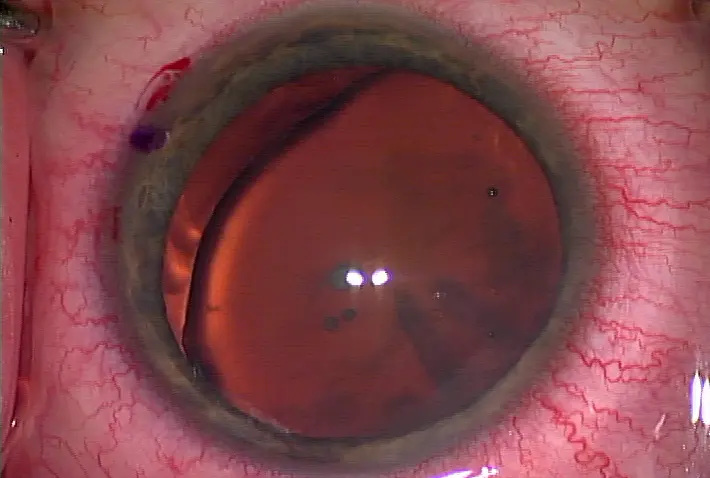
I fix the lens by filling the anterior chamber with viscoelastic material and orient it by using the red reflex of the light of the microscope at the level of the cornea and lens. In this way, perfect centration is obtained with regard to the optical axis of the patient because he or she is going to look at a light that is present in the microscope itself. This lens has no support at the level of the periphery of the capsular bag but is supported by the capsular bag, which means there is another dimension of freedom in that the surgeon can position the lens where it is optically optimal. This makes it possible for complex optics like aspherical lenses, toric lenses, and multifocal lenses to be positioned according to the optical axis of the patient, not according to the anatomical parameters of the eye like it is currently done in the traditional lens-in-the-bag implantation technique. So far, our study, which follows clinical trial guidelines of Belgium's equivalent of the FDA, has evaluated 4,000 patients who have undergone the procedure using this lens. We now have 10 years' worth of follow-up that shows 100% no PCO in adult eyes and excellent results with the lens.
A standard bag-in-the-lens implant Source: Marie-Jose Tassignon, M.D., Ph.D.
A toric bag-in-the-lens implant Source: Marie-Jose Tassignon, M.D., Ph.D
Bag-in-the-lens with complex optics
I recently began to explore the procedure using complex optics and have finished a study on toric lenses. Colleagues and I studied 52 eyes of patients who had up to 8 D of astigmatism correction. Our experience is with about 70 eyes that have been implanted. We found that the BIL procedure works with toric IOLs as well, and we are now developing multifocal IOLs to be positioned according to the optical axis of the patient. While this work is still in its early stages, I have combined the bag-in-the-lens with an add-on lens that is a multifocal and have discovered mixed reactions from patients—some are relatively happy with the results and some are not happy with the combination. The reason is the centration of the bag-in-the-lens is based on the optical axis of the patient while the centration of the add-on lens is based on the ciliary sulcus of the patient, and those are not necessarily completely aligned. I now use a kind of index of geometrical center of the limbus. If the geometrical center fits the center of the papillary entrance of the patient, then the patient will be happy with the add-on multifocal lens; otherwise the patient will have complaints. The new approach to predicting happy patients with complex lenses is therefore paying attention to the pupillary axis of the eye.
Pearls to getting it right
The learning curve in my observation is the younger the surgeon, the easier it is for him or her to learn. Older ophthalmologists have a little bit of difficulty because it's a different approach from what they're used to. There are some crucial aspects of the procedure that surgeons need to take note of. For example, because both capsules have to be positioned within the groove of the lens after having done anterior and posterior capsulorhexis, both capsules have to stay very close to each other; otherwise, the surgeon is never going to get both capsules within the groove. Surgeons must perform posterior continuous curvilinear capsulorhexis according to very precise protocol, perforating the posterior capsule only when the capsule is in the horizontal position. The risk of harming the anterior hyaloids is lower when the capsule is loose in the horizontal position instead of bent posteriorly with a filled capsular bag. In addition, never fill the capsular bag after having emptied it of its contents. I always perform the procedure under topical anesthesia; this way, the vitreous has no pressure and the eye is very quiet. I have had no incidences of vitreous loss. Potential complications of the procedure are the same as that of the traditional lens-in-the-bag implantation technique. The reason I use this technique routinely is because the posterior capsule is absent, allowing full transparency of the anterior segment of the eye and avoiding forward scatter of the incoming light completely. The lens can still be improved, of course, as can the lenses used in the traditional implantation technique. However, if optimal quality of vision is the goal, it cannot be obtained with classic lens implantation because patients will find decreases in visual acuity or contrast sensitivity with time as the capsular bag becomes more opaque due to conditions such as fibrotic reaction, capsular contraction, and proliferation of the lens epithelial cells.
Further developments
I'm currently developing the bag-in-the-lens technique to work where there is no capsule by creating an artificial capsule that can be positioned at the level of the sclera, and the bag-in-the-lens can be inserted in the middle.
Editors' note: The bag-in-the-lens is approved for use in Europe and is undergoing trials for FDA approval in the U.S. Dr. Tassignon has a proprietary interest in the bag-in-the-lens IOL.
Contact information
Tassignon: +32 3821 3377, marie-jose.tassignon@uza.be


留言
張貼留言