August 2011‧Eye World
Evaluating patients for premium IOLs
by Enette Ngoei EyeWorld Contributing Editor
EyeWorld talks to experts about the extra measures they take when evaluating premium IOL patients
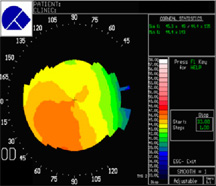 |
| Topography scans are common scans used in evaluating patients for IOLs Source: David T.C. Lin, M.D. |
Dry eye tests, topography tests, and OCT scans—with high patient expectations of gaining complete spectacle independence following premium lens surgery, detailed pre-op evaluations are needed to ensure optimal outcomes.
Lisa Tsai, M.D., assistant professor, ophthalmology and visual sciences, Washington University School of Medicine, St. Louis, said her pre-op evaluation for premium lens patients closely resembles what she does for patients undergoing LASIK surgery. First, Dr. Tsai conducts a full ocular exam, including an assessment of uncorrected vision at distance and near. "Even if [patients] wear glasses, it's important to document that with a full exam," she said.
She measures pupil size and does BAT testing for glare problems. On the initial exam, she may not always do the Schirmer's test, although she is starting to do it more for her dry eye patients, she said.
Dr. Tsai also performs a good retina exam, and if there are any concerns, she'll do an Amsler Grid exam in the office. Although she currently doesn't do an OCT scan on all of her patients, she is thinking of going that way.
Patients with the potential for and interest in getting premium IOL implants are then put on Restasis (cyclosporine, Allergan, Irvine, Calif.) or a lubricant drop and are asked to come back for pre-op measurements, Dr. Tsai said.
"I want to make sure that I can double check my measurements, particularly the astigmatism," she explained.
During the second round of measurements, Dr. Tsai rechecks the manual keratometry readings and does topography on all of her patients. "If it hasn't been done, I'll do pupil size and redo the A-scan at that time so when I'm looking at astigmatism I've got the K measurements from the initial exam and then I've got repeat Ks, topography, and A-scan from the day that the patient came back," she said.
Dr. Tsai always checks the dominant eye because she wants to see how vision is going to be integrated in the patient's whole system, she explained. Another essential part of her pre-op exam is the Vision Assessment Questionnaire developed by Steven Dell, M.D. Dr. Tsai currently offers the Crystalens AO or HD (Bausch & Lomb, Rochester, N.Y.) and the Tecnis Multifocal IOL (Abbott Medical Optics, Santa Ana, Calif.), and the questionnaire helps her determine which one of those implants might be more accommodating for the patient, she explained.
All the time or some of the time?
Apart from thorough ocular exams, some experts recommend corneal topography mapping as well as OCT scans for all premium IOL patients. Both Dr. Tsai and Leslie Brannon Aden, M.D., Mississippi Vision Correction Center, Flowood, perform topographies on all their premium IOL patients. But when it comes to OCT scans, neither are doing them all of the time. Looking for underlying corneal pathology and making sure to rule out any type of possible keratoconus is important, Dr. Tsai said. While some practices might not have access to a topography machine, it is becoming the standard of care, she said.
On the other hand, OCTs and the imaging of the retina are more difficult to have access to, Dr. Tsai said. She did not have the equipment readily available before, but now that she does, she said it doesn't hurt to have more information that you can share with the patient ahead of time, to show that you spent extra time looking for any abnormalities that could affect the outcome.
Patients can sometimes develop retinal pathology like an epiretinal membrane following multifocal IOL implantation, so it is good to be able to show them this was not something that they had before and that they were a good candidate for premium lenses at the time of surgery.
Dr. Aden thinks that while the OCT is appropriate in a lot of premium IOL patients, she doesn't believe it's necessary in 100% of the cases. She draws the distinction between multifocal lenses and toric lenses.
The toric lens is not as dependent upon the retina being perfectly healthy to function in the way it should, Dr. Aden explained.
"I will put a toric lens in a patient who has retinal pathology if the patient has astigmatism and wants to be free from wearing prescription lenses for distance. I don't think there's a contraindication there because that patient will have to wear glasses for the correction of astigmatism anyway."
But she wouldn't put a multifocal IOL in a patient with macular pathology who does not have astigmatism and wants a multifocal lens. In such an instance, it takes an OCT to identify that the macular pathology is there.
In terms of measuring axial length, both surgeons prefer the IOLMaster (Carl Zeiss Meditec, Dublin, Calif.). If there are any questions about her IOL measurements, however, Dr. Tsai said she will use the immersion technique.
Both surgeons use corneal marking instruments for their toric patients. Dr. Tsai said she uses them for her multifocal IOL patients if she's doing a peripheral corneal relaxing incision. Dr. Aden said she sometimes uses them to determine the center of the visual axis if she is concerned about where the visual axis is in order to align a multifocal lens properly. Neither uses an intraoperative aberrometer. While Dr. Aden said there are certain circumstances where it would be useful, she has found her own results consistent enough that she doesn't have a need for it.
Providing appropriate patient counseling
When it comes to what a physician's ethical responsibility is, Dr. Tsai said treating all patients like they've come in for a cataract removal, without leaping to the part where they are offered a premium IOL, is important to her.
"Whether or not they want a premium IOL, I would treat them like any other pre-op patients and give them all the risks and benefits of the surgery, and I definitely offer them the option of a premium IOL as well as a standard IOL," she said.
It's important to offer both options even though some practices may feel strongly about the premium IOLs, Dr. Tsai said, as she thinks of it as a personal choice for the patient. Patients who come in asking for premium lenses may not understand all the benefits and risks they entail; it's a physician's duty to take the extra time to explain so patients understand and have reasonable expectations, Dr. Tsai said.
If the patient decides to go with a premium IOL, then doing extra testing like Schirmer's, topography, and BAT testing to maximize the outcome for the patient is an ethical responsibility.
On the other hand, if the surgeon knows the patient will not do well with a certain technology, the ethical responsibility is on the physician to make the choice against this technology, Dr. Aden said.
Another ethical concern is that as soon as patients decide to pay out of pocket, the way they are treated changes. Dr. Tsai said that the only thing that she thinks should change is the extra time she spends counseling patients to get a better outcome.
How much testing is enough?
Surgeons can run the risk of throwing a lot of testing at patients without having a clinical plan, Dr. Tsai said.
"Testing by itself is not a substitute for having a clinical picture in mind of some of the issues that you're concerned about and having a discussion with the patient using the results of the tests," Dr. Tsai said.
Although she thinks how much testing is enough varies from one patient to another, Dr. Aden said premium lens patients have to have a definitive evaluation of astigmatism, which may mean topography at the very least and, in her opinion, other methods of confirming and verifying that the astigmatism is measuring in the same way because it has to be addressed. In her clinic, ruling out the possibility of any abnormalities in the visual system that could potentially interfere with the function of the lens means she does an OCT on some patients and uses, at minimum, an IOLMaster, a Lenstar (Haag-Strait, Mason, Ohio), or an immersion technique as the standard of care, Dr. Aden said.
Editors' note: Drs. Aden and Tsai have no financial interests related to their comments.
Contact information
Aden: 601-969-1430, contact@mississippivision.com
Tsai: 314-362-3937, tsai@vision.wustl.edu




留言
張貼留言