Linking keratoconus and floppy eyelid syndrome to sleep apnea
Linking keratoconus and floppy eyelid syndrome to sleep apnea


An example of FES Source: Francis S. Mah, M.D.

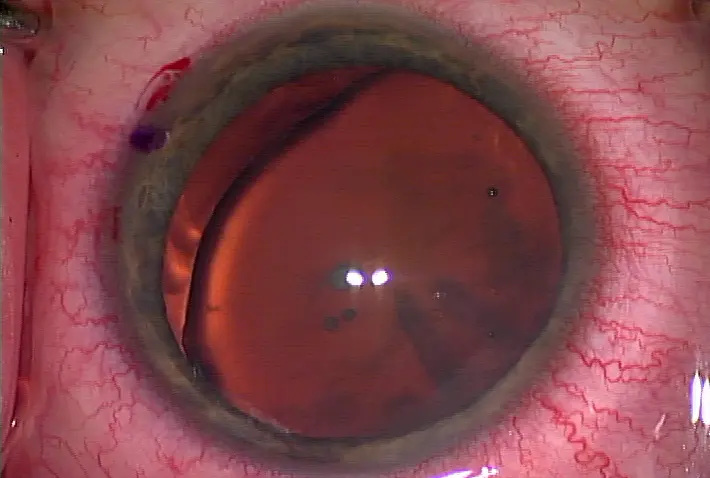
A patient with keratoconus Source: Uday Devgan, M.D.
Does your patient need a sleep study?
Has a patient ever nodded off in the exam chair or perhaps mentioned problems sleeping? Does that patient have keratoconus or floppy eyelid syndrome (FES)? If so, pay attention. Keratoconus and FES are linked to sleep apnea, a dangerous sleep disorder characterized by breaks in breathing that's associated with heart disease, stroke, hypertension, atrial fibrillation, congestive heart failure, and other deadly vascular diseases. Keratoconus, FES, and sleep apnea exist independently of each other. For example, many keratoconus patients don't have sleep apnea, and many sleep apnea patients don't have keratoconus. But it's not unusual to find a keratoconus or FES patient with sleep apnea. What are the signs and symptoms of sleep apnea, keratoconus, and FES? And if having one doesn't guarantee the development of the other, how are they linked?
Signs and symptoms
The signs and symptoms of sleep apnea are pretty well defined. They include daytime sleepiness, falling asleep while driving, and excessive snoring. The disease affects more men than women, and the National Institutes of Health estimates 1 out of 10 adults 65 and older have sleep apnea. "There's a huge epidemic of sleep apnea," said Michael A. Saidel, M.D., director, Cornea Service, University of Chicago. "It's a major problem in the United States. It's associated with obesity and with all causes of morbidity and mortality. It's a horrible disease." Keratoconus is a disease of young people and is characterized by central cornea thinning, causing the cornea to develop a cone shape. Symptoms include blurred vision and light sensitivity. "The cornea is like a bunch of layers of spaghetti, and the spaghetti has bonds between the multiple layers," explained Charles Bouchard, M.D., John P. Mulcahy Professor of Ophthalmology, and chairman, Ophthalmology, Loyola University, Chicago. "In keratoconus, there seems to be a decrease in the number of cells in the cornea and some elevation in inflammatory cytokines or inflammatory mediators. The thought is that over time, these collagen spaghetti fibers slide over each other and create that abnormal conical shape." Like sleep apnea, FES is most frequently seen in overweight males. It's caused by a decrease in elastin in the eyelids, which allows the eyelids to be easily turned upward and become floppy. FES severity and symptoms exist on a spectrum and can range from ocular redness and irritation to corneal ulcer. "There's a lot of people in between who have the disease, but it's under recognized because it's not symptomatic," Dr. Saidel said.
What links them together?
The link between sleep apnea, keratoconus, and FES is known, but not well understood. A quick search on PubMed reveals a multitude of studies linking FES and keratoconus to sleep apnea, but nothing hones in on one reason in particular. The diseases do have one common dominator: decreased elasticity and abnormal collagen. "With sleep apnea, there's abnormal collagen and elasticity, and with keratoconus there's a collagen problem," Dr. Bouchard said. "And with floppy eyelid syndrome there's certainly alternation in elastic and collagen in the eyelids. The three diseases are linked by an abnormality in collagen." Regretfully, curing sleep apnea won't help with the patient's FES or keratoconus. And of course, just because a patient has keratoconus or FES doesn't mean he or she will develop sleep apnea. Drs. Bouchard and Saidel, however, do recommend screening all patients with FES and keratoconus for sleep apnea. "All keratoconus and floppy eyelid patients should be asked if they have trouble sleeping," Dr. Bouchard said. "Sleep apnea should be on the list of suspicious associated diseases that general ophthalmologists should be aware of. If they see keratoconus, they should think sleep apnea and ask the patient about it."
Issues to go over with the patient include daytime sleepiness, prevalence of falling asleep at the wheel, and overall sleep hygiene. Obesity and dozing off in the exam chair are other tipoffs. "With those two things you should be very suspicious of sleep apnea and refer them for further testing," Dr. Saidel said. "You can't make the diagnosis of sleep apnea without having patients show they've had an episode of sleep apnea. This is typically done with a nighttime polysomnogram."
Once identified, sleep apnea is treatable with continuous positive airway pressure therapy. Patients wear a mask attached to a hose and machine when sleeping that supplies a continuous stream of air, thus preventing apnea. "Sleep apnea is a serious disease," Dr. Bouchard said. "[Patients] could die. The general ophthalmologist should be aware of the association of sleep apnea, keratoconus, and floppy eyelid syndrome because patients may need a referral to a sleep study to confirm that."
Editors' note: The doctors mentioned have no financial interests related to this article.
Contact information
Bouchard: cboucha@lumc.edu
Saidel: msaidel@bsd.uchicago.edu
by Faith A. Hayden EyeWorld Staff Writer
An example of FES Source: Francis S. Mah, M.D.
A patient with keratoconus Source: Uday Devgan, M.D.
Does your patient need a sleep study?
Has a patient ever nodded off in the exam chair or perhaps mentioned problems sleeping? Does that patient have keratoconus or floppy eyelid syndrome (FES)? If so, pay attention. Keratoconus and FES are linked to sleep apnea, a dangerous sleep disorder characterized by breaks in breathing that's associated with heart disease, stroke, hypertension, atrial fibrillation, congestive heart failure, and other deadly vascular diseases. Keratoconus, FES, and sleep apnea exist independently of each other. For example, many keratoconus patients don't have sleep apnea, and many sleep apnea patients don't have keratoconus. But it's not unusual to find a keratoconus or FES patient with sleep apnea. What are the signs and symptoms of sleep apnea, keratoconus, and FES? And if having one doesn't guarantee the development of the other, how are they linked?
Signs and symptoms
The signs and symptoms of sleep apnea are pretty well defined. They include daytime sleepiness, falling asleep while driving, and excessive snoring. The disease affects more men than women, and the National Institutes of Health estimates 1 out of 10 adults 65 and older have sleep apnea. "There's a huge epidemic of sleep apnea," said Michael A. Saidel, M.D., director, Cornea Service, University of Chicago. "It's a major problem in the United States. It's associated with obesity and with all causes of morbidity and mortality. It's a horrible disease." Keratoconus is a disease of young people and is characterized by central cornea thinning, causing the cornea to develop a cone shape. Symptoms include blurred vision and light sensitivity. "The cornea is like a bunch of layers of spaghetti, and the spaghetti has bonds between the multiple layers," explained Charles Bouchard, M.D., John P. Mulcahy Professor of Ophthalmology, and chairman, Ophthalmology, Loyola University, Chicago. "In keratoconus, there seems to be a decrease in the number of cells in the cornea and some elevation in inflammatory cytokines or inflammatory mediators. The thought is that over time, these collagen spaghetti fibers slide over each other and create that abnormal conical shape." Like sleep apnea, FES is most frequently seen in overweight males. It's caused by a decrease in elastin in the eyelids, which allows the eyelids to be easily turned upward and become floppy. FES severity and symptoms exist on a spectrum and can range from ocular redness and irritation to corneal ulcer. "There's a lot of people in between who have the disease, but it's under recognized because it's not symptomatic," Dr. Saidel said.
What links them together?
The link between sleep apnea, keratoconus, and FES is known, but not well understood. A quick search on PubMed reveals a multitude of studies linking FES and keratoconus to sleep apnea, but nothing hones in on one reason in particular. The diseases do have one common dominator: decreased elasticity and abnormal collagen. "With sleep apnea, there's abnormal collagen and elasticity, and with keratoconus there's a collagen problem," Dr. Bouchard said. "And with floppy eyelid syndrome there's certainly alternation in elastic and collagen in the eyelids. The three diseases are linked by an abnormality in collagen." Regretfully, curing sleep apnea won't help with the patient's FES or keratoconus. And of course, just because a patient has keratoconus or FES doesn't mean he or she will develop sleep apnea. Drs. Bouchard and Saidel, however, do recommend screening all patients with FES and keratoconus for sleep apnea. "All keratoconus and floppy eyelid patients should be asked if they have trouble sleeping," Dr. Bouchard said. "Sleep apnea should be on the list of suspicious associated diseases that general ophthalmologists should be aware of. If they see keratoconus, they should think sleep apnea and ask the patient about it."
Issues to go over with the patient include daytime sleepiness, prevalence of falling asleep at the wheel, and overall sleep hygiene. Obesity and dozing off in the exam chair are other tipoffs. "With those two things you should be very suspicious of sleep apnea and refer them for further testing," Dr. Saidel said. "You can't make the diagnosis of sleep apnea without having patients show they've had an episode of sleep apnea. This is typically done with a nighttime polysomnogram."
Once identified, sleep apnea is treatable with continuous positive airway pressure therapy. Patients wear a mask attached to a hose and machine when sleeping that supplies a continuous stream of air, thus preventing apnea. "Sleep apnea is a serious disease," Dr. Bouchard said. "[Patients] could die. The general ophthalmologist should be aware of the association of sleep apnea, keratoconus, and floppy eyelid syndrome because patients may need a referral to a sleep study to confirm that."
Editors' note: The doctors mentioned have no financial interests related to this article.
Contact information
Bouchard: cboucha@lumc.edu
Saidel: msaidel@bsd.uchicago.edu


留言
張貼留言