Complicated cataract cases Cataract surgery in patients with Fuchs' dystrophy
Complicated cataract cases
Cataract surgery in patients with Fuchs' dystrophy
--------------------------------------------------------------------------------
Fuchs' dystrophy is the most common endothelial dystrophy affecting human corneas. Cataract is the most common ailment affecting the eye of older adults. The intersection of these two problems in the same eye is not uncommon.
Many patients with cataract have mild to moderate guttata and stromal thickening at the time of cataract evaluation. In many cases it is not clear whether cataract or Fuchs' dystrophy contributes more to the decline in vision. Clinical judgment and experience are necessary to distinguish between the contributions. Sometimes it isn't known until after surgical intervention.
In recent years, endothelial keratoplasty (DSAEK, DSEK, DMEK) replaced penetrating keratoplasty as the most common surgical procedure for treating advanced Fuchs' corneal endothelial dystrophy. Endothelial keratoplasty has significant advantages with respect to recovery time; reduced comorbidity, especially astigmatism; and easier decision-making with regard to combined surgery as compared to penetrating keratoplasty. Its disadvantages are a hyperopic shift in post-op refraction if significant stromal tissue remains on the graft (DSAEK, DSEK) and a slightly reduced corrected visual acuity. The latter problem seems to have been resolved in large measure by eliminating most or all of the stromal tissue (DMEK).
The fundamental decision that a cataract surgeon must make is whether to perform cataract surgery alone, endothelial keratoplasty alone, or combined surgery. Simple metrics provide general guidelines but do not predict the behavior of every eye. Clinical factors such as a history of early morning blurred vision and a finding of subtle Descemet's striae often influence the decision-making process, regardless of the numbers.
Cataract surgery is safer than it used to be. Advanced phaco technologies, excellent dispersive and viscoadaptive OVDs, soft shell techniques, and advanced fluidics have lowered the rate of endothelial cell injury and loss. Operating on patients with Fuchs' dystrophy is not as traumatic as it would have been just a few years ago.
In this issue, Brian Alder, M.D., and Terry Kim, M.D., discuss the decision-making process for eyes with Fuchs' dystrophy. They also discuss intraoperative and post-op considerations when combined surgery is performed.
Kevin Miller, M.D., Complicated cataract cases editor
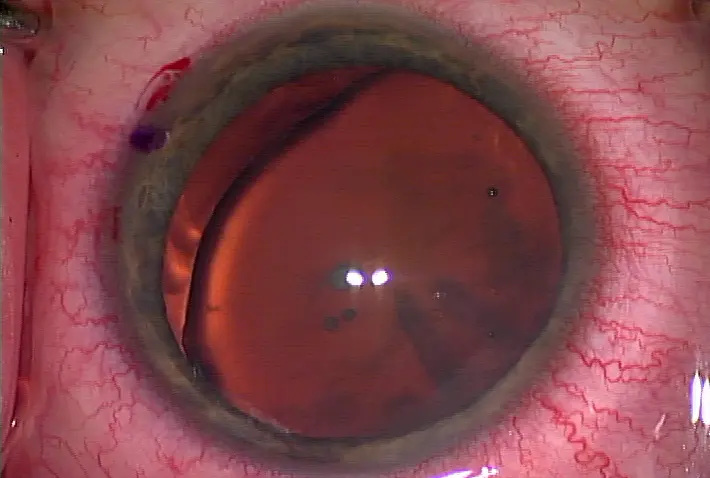
Figure 1. Patient with significant corneal endothelial guttae on slit lamp examination
Figure 2. Patient with advanced Fuchs' dystrophy and endothelial cell loss on specular microscopy
Figure 3. Example of chop technique and OZil torsional phacoemulsification (Alcon) settings to decrease corneal endothelial damage during cataract extraction Source (all): Brian Alder, M.D., and Terry Kim, M.D.
Patients with Fuchs' corneal endothelial dystrophy and cataract can present a unique challenge to the ophthalmologist. While many such patients have a visually significant cataract and Fuchs' dystrophy and clearly require combined cataract extraction with endothelial transplant, there are situations where one may proceed with either cataract surgery or Descemet's stripping automated endothelial keratoplasty (DSAEK) surgery alone. Here we will present our views on clinical settings wherein cataract surgery may be performed without endothelial transplant, as well as focus on several surgical techniques that may aid in a successful outcome. Finally, we discuss several post-op recommendations specific to the patient with mild Fuchs' dystrophy who has undergone cataract extraction.
Decision-making: Cataract extraction alone or combined DSAEK surgery?
everal factors must be considered when evaluating a patient with both cataract and Fuchs' dystrophy. A primary consideration for such patients is the severity and degree of each disease process present. If a patient has significant guttae on exam, documented increasing pachymetry or significant asymmetry on pachymetry, or any evidence of epithelial edema, we recommend proceeding with combined cataract extraction and endothelial transplant. In addition, if patients report a history of morning blurry vision that clears over the day, consistent with microcystic edema from Fuchs' dystrophy, despite a mild appearance on exam, strong consideration should be given to proceeding with a combined surgery.
Another key consideration is the patient's visual demand. Recommendations may differ for the 55-year-old requiring a high degree of visual acuity for many years and the 90-year-old who would like to regain some reading vision. Similarly, one must consider a patient's ability to provide necessary post-op care for a transplant for an extended period of time compared to post-op cataract care.
For patients with visually significant cataracts but with mild guttae and minimal stromal corneal edema on exam, it's reasonable to proceed with cataract surgery alone, with special attention given to surgical technique as described below so as to minimize traumatic injury to the already diseased corneal endothelium.
Surgical technique
Viscoelastic selection: Protection of the corneal endothelium is of paramount importance in patients with mild Fuchs' dystrophy undergoing cataract surgery. One important way to minimize endothelial trauma is to use a dispersive viscoelastic (e.g., Viscoat, Alcon, Fort Worth, Texas, or Healon D, Abbott Medical Optics, Santa Ana, Calif.) during phacoemulsification. With shorter side chains and lower viscosity, such viscoelastics easily disperse throughout the anterior chamber after injection, providing a true protective coating to the corneal endothelium that lasts longer than cohesive viscoelastics during the operative procedure. This protective coating serves as a mechanical barrier to excessive ultrasound energy and trauma during phacoemulsification that may otherwise harm the corneal endothelium.
Special attention should also be given to removing dispersive viscoelastics from the anterior chamber after phacoemulsification. For the same reasons that they provide a protective coating to the endothelium, these viscoelastics tend to adhere to the endothelium, and if thorough aspiration and irrigation of the anterior chamber is not performed, the patient may be at increased risk of a post-op rise in IOP related to retained viscoelastic obstructing aqueous outflow.
Phaco technique and technology: Specific phacoemulsification techniques may also play a role in the amount of energy produced and resultant trauma to the corneal endothelium. In general, we recommend using a phaco-chop technique rather than a divide and conquer technique. In our experience, this technique allows for less phaco power and phaco time necessary for cataract extraction. Wong et al performed a prospective, randomized study comparing phaco time and phaco power between the two techniques and found similar results.1 In addition, we recommend using advanced phacoemulsification technologies (i.e., torsional or transversal ultrasound), which offer the benefits of increased efficiency in lens removal, greatly reduced repulsion of lens material from the tip, decreased turbulence in the anterior chamber, enhanced followability of lens material, and less risk of thermal corneal wound burns.
We have previously published results showing overall less cumulative dissipated energy and less endothelial cell loss when a torsional handpiece was used through a 2.2 mm micro-incision compared to a 2.8 mm standard technique.2
Post-op considerations
A patient with mild Fuchs' corneal dystrophy who has undergone cataract surgery alone should be followed carefully in the post-op period to ensure clearing of any surgery-related corneal edema. These patients benefit from more frequent steroid use or use of a more potent steroid (i.e., difluprednate 0.05%). In addition, we occasionally give these patients topical hyperosmotic agents (e.g., sodium chloride hypertonicity ophthalmic solution 5% and ointment) in the early post-op period to expedite and ensure deturgescence of the cornea.
Conclusions
In summary, while DSAEK surgery provides safe and predictable outcomes for patients with Fuchs' dystrophy, there are certain clinical scenarios where we may consider cataract surgery alone in a patient with mild Fuchs' dystrophy. When we do proceed with cataract surgery in such patients, we plan our surgical technique and utilize advanced phacoemulsification technologies in order to minimize corneal endothelial trauma and maximize endothelial protection so that the best visual outcomes can be offered to our patients.
References
1. Wong T, Hingorani M, Lee V. Phacoemulsification time and power requirements in phaco chop and divide and conquer nucleofractis techniques. J Cataract Refract Surg 2000; 26:1374-1378.
2. Berhahl JP, Jun BK, DeStafeno JJ, Kim T. Comparison of a Torsional Handpiece Through Microincision Versus Standard Clear Corneal Cataract Wounds. J Cataract Refract Surg 2008; 34(12): 2091-2095.
Editors' note: Dr. Kim is professor of ophthalmology, cornea and refractive surgery, Duke University Eye Center, Durham, N.C. He has financial interests with Alcon. Dr. Alder is chief resident, Duke University Eye Center. He has no financial interests related to the article.
Contact information
Alder: brian.alder@duke.edu
Kim: terry.kim@duke.edu
Cataract surgery in patients with Fuchs' dystrophy
--------------------------------------------------------------------------------
by Brian Alder, M.D., and Terry Kim, M.D.
Fuchs' dystrophy is the most common endothelial dystrophy affecting human corneas. Cataract is the most common ailment affecting the eye of older adults. The intersection of these two problems in the same eye is not uncommon.
Many patients with cataract have mild to moderate guttata and stromal thickening at the time of cataract evaluation. In many cases it is not clear whether cataract or Fuchs' dystrophy contributes more to the decline in vision. Clinical judgment and experience are necessary to distinguish between the contributions. Sometimes it isn't known until after surgical intervention.
In recent years, endothelial keratoplasty (DSAEK, DSEK, DMEK) replaced penetrating keratoplasty as the most common surgical procedure for treating advanced Fuchs' corneal endothelial dystrophy. Endothelial keratoplasty has significant advantages with respect to recovery time; reduced comorbidity, especially astigmatism; and easier decision-making with regard to combined surgery as compared to penetrating keratoplasty. Its disadvantages are a hyperopic shift in post-op refraction if significant stromal tissue remains on the graft (DSAEK, DSEK) and a slightly reduced corrected visual acuity. The latter problem seems to have been resolved in large measure by eliminating most or all of the stromal tissue (DMEK).
The fundamental decision that a cataract surgeon must make is whether to perform cataract surgery alone, endothelial keratoplasty alone, or combined surgery. Simple metrics provide general guidelines but do not predict the behavior of every eye. Clinical factors such as a history of early morning blurred vision and a finding of subtle Descemet's striae often influence the decision-making process, regardless of the numbers.
Cataract surgery is safer than it used to be. Advanced phaco technologies, excellent dispersive and viscoadaptive OVDs, soft shell techniques, and advanced fluidics have lowered the rate of endothelial cell injury and loss. Operating on patients with Fuchs' dystrophy is not as traumatic as it would have been just a few years ago.
In this issue, Brian Alder, M.D., and Terry Kim, M.D., discuss the decision-making process for eyes with Fuchs' dystrophy. They also discuss intraoperative and post-op considerations when combined surgery is performed.
Kevin Miller, M.D., Complicated cataract cases editor
Figure 1. Patient with significant corneal endothelial guttae on slit lamp examination
Figure 2. Patient with advanced Fuchs' dystrophy and endothelial cell loss on specular microscopy
Figure 3. Example of chop technique and OZil torsional phacoemulsification (Alcon) settings to decrease corneal endothelial damage during cataract extraction Source (all): Brian Alder, M.D., and Terry Kim, M.D.
Patients with Fuchs' corneal endothelial dystrophy and cataract can present a unique challenge to the ophthalmologist. While many such patients have a visually significant cataract and Fuchs' dystrophy and clearly require combined cataract extraction with endothelial transplant, there are situations where one may proceed with either cataract surgery or Descemet's stripping automated endothelial keratoplasty (DSAEK) surgery alone. Here we will present our views on clinical settings wherein cataract surgery may be performed without endothelial transplant, as well as focus on several surgical techniques that may aid in a successful outcome. Finally, we discuss several post-op recommendations specific to the patient with mild Fuchs' dystrophy who has undergone cataract extraction.
Decision-making: Cataract extraction alone or combined DSAEK surgery?
everal factors must be considered when evaluating a patient with both cataract and Fuchs' dystrophy. A primary consideration for such patients is the severity and degree of each disease process present. If a patient has significant guttae on exam, documented increasing pachymetry or significant asymmetry on pachymetry, or any evidence of epithelial edema, we recommend proceeding with combined cataract extraction and endothelial transplant. In addition, if patients report a history of morning blurry vision that clears over the day, consistent with microcystic edema from Fuchs' dystrophy, despite a mild appearance on exam, strong consideration should be given to proceeding with a combined surgery.
Another key consideration is the patient's visual demand. Recommendations may differ for the 55-year-old requiring a high degree of visual acuity for many years and the 90-year-old who would like to regain some reading vision. Similarly, one must consider a patient's ability to provide necessary post-op care for a transplant for an extended period of time compared to post-op cataract care.
For patients with visually significant cataracts but with mild guttae and minimal stromal corneal edema on exam, it's reasonable to proceed with cataract surgery alone, with special attention given to surgical technique as described below so as to minimize traumatic injury to the already diseased corneal endothelium.
Surgical technique
Viscoelastic selection: Protection of the corneal endothelium is of paramount importance in patients with mild Fuchs' dystrophy undergoing cataract surgery. One important way to minimize endothelial trauma is to use a dispersive viscoelastic (e.g., Viscoat, Alcon, Fort Worth, Texas, or Healon D, Abbott Medical Optics, Santa Ana, Calif.) during phacoemulsification. With shorter side chains and lower viscosity, such viscoelastics easily disperse throughout the anterior chamber after injection, providing a true protective coating to the corneal endothelium that lasts longer than cohesive viscoelastics during the operative procedure. This protective coating serves as a mechanical barrier to excessive ultrasound energy and trauma during phacoemulsification that may otherwise harm the corneal endothelium.
Special attention should also be given to removing dispersive viscoelastics from the anterior chamber after phacoemulsification. For the same reasons that they provide a protective coating to the endothelium, these viscoelastics tend to adhere to the endothelium, and if thorough aspiration and irrigation of the anterior chamber is not performed, the patient may be at increased risk of a post-op rise in IOP related to retained viscoelastic obstructing aqueous outflow.
Phaco technique and technology: Specific phacoemulsification techniques may also play a role in the amount of energy produced and resultant trauma to the corneal endothelium. In general, we recommend using a phaco-chop technique rather than a divide and conquer technique. In our experience, this technique allows for less phaco power and phaco time necessary for cataract extraction. Wong et al performed a prospective, randomized study comparing phaco time and phaco power between the two techniques and found similar results.1 In addition, we recommend using advanced phacoemulsification technologies (i.e., torsional or transversal ultrasound), which offer the benefits of increased efficiency in lens removal, greatly reduced repulsion of lens material from the tip, decreased turbulence in the anterior chamber, enhanced followability of lens material, and less risk of thermal corneal wound burns.
We have previously published results showing overall less cumulative dissipated energy and less endothelial cell loss when a torsional handpiece was used through a 2.2 mm micro-incision compared to a 2.8 mm standard technique.2
Post-op considerations
A patient with mild Fuchs' corneal dystrophy who has undergone cataract surgery alone should be followed carefully in the post-op period to ensure clearing of any surgery-related corneal edema. These patients benefit from more frequent steroid use or use of a more potent steroid (i.e., difluprednate 0.05%). In addition, we occasionally give these patients topical hyperosmotic agents (e.g., sodium chloride hypertonicity ophthalmic solution 5% and ointment) in the early post-op period to expedite and ensure deturgescence of the cornea.
Conclusions
In summary, while DSAEK surgery provides safe and predictable outcomes for patients with Fuchs' dystrophy, there are certain clinical scenarios where we may consider cataract surgery alone in a patient with mild Fuchs' dystrophy. When we do proceed with cataract surgery in such patients, we plan our surgical technique and utilize advanced phacoemulsification technologies in order to minimize corneal endothelial trauma and maximize endothelial protection so that the best visual outcomes can be offered to our patients.
References
1. Wong T, Hingorani M, Lee V. Phacoemulsification time and power requirements in phaco chop and divide and conquer nucleofractis techniques. J Cataract Refract Surg 2000; 26:1374-1378.
2. Berhahl JP, Jun BK, DeStafeno JJ, Kim T. Comparison of a Torsional Handpiece Through Microincision Versus Standard Clear Corneal Cataract Wounds. J Cataract Refract Surg 2008; 34(12): 2091-2095.
Editors' note: Dr. Kim is professor of ophthalmology, cornea and refractive surgery, Duke University Eye Center, Durham, N.C. He has financial interests with Alcon. Dr. Alder is chief resident, Duke University Eye Center. He has no financial interests related to the article.
Contact information
Alder: brian.alder@duke.edu
Kim: terry.kim@duke.edu






The Alcon IpGuide LASIK Handpiece is an ideal choice for a patient who has undergone cataract surgery. Its smooth removal of the cortex, capsular-friendly tip, and stability make this an excellent option for LASIK surgery. Learn more about ellips fx handpiece on ophthalmon.com.
回覆刪除