Cornea editor's corner of the world Treating ocular surface squamous neoplasia
Cornea editor's corner of the world
Treating ocular surface squamous neoplasia
--------------------------------------------------------------------------------
Ocular surface squamous neoplasia (OSSN) is not a common condition but is one that all clinicians need to be able to recognize. An early diagnosis with a small lesion results in a very good prognosis. However, a delay in diagnosis can lead to a lesion that involves a large area of epithelium including a significant amount of the limbal stem cells and conjunctival. Treating these larger lesions is more difficult and has a higher recurrence rate. All clinicians should be aware of the clinical findings of OSSN: irregular, thickened limbal, corneal and conjunctival epithelium, and neovascularization. The abnormal epithelium typically arises from the limbus and can progress centrally over the cornea or posteriorly over the conjunctiva or in both directions. An atypical "pterygium" in an elderly patient should alert one to the diagnosis of OSSN.
Many new adjunct treatments are now available to reduce the recurrence and avoid the problem of multiple excisions in those cases of recurrence. Mitomycin-C (MMC), 5-fluorouracil (5-FU), and interferon alpha 2b are all adjunctive treatment choices in addition to the standard surgical resection and cryotherapy. In this issue's "Cornea corner of the world," Carol L. Karp, M.D., and Shahzad I. Mian, M.D., share their insights into the management of OSSN.
Edward J. Holland, M.D., cornea editor
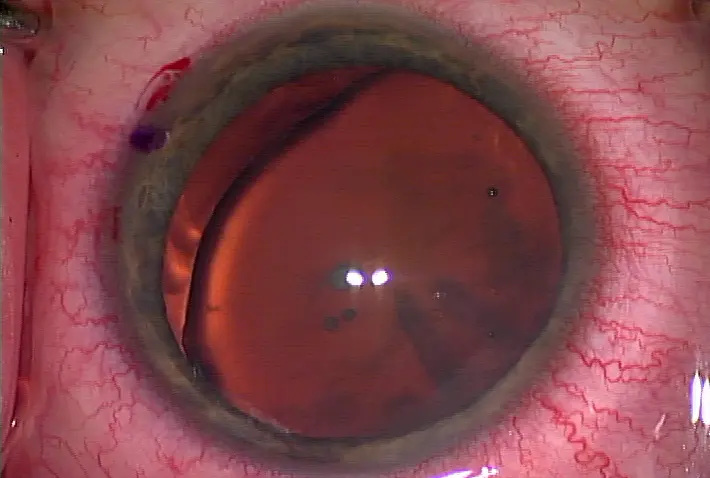
A gelatinous-appearing ocular surface squamous neoplasia
Ocular surface squamous neoplasia in an HIV-positive patient. Note feeder vessels and both papillary and leukoplakic features of the lesion Source (all): Carol L. Karp, M.D.
This disease rarely metastasizes, but it can cause severe tissue destruction
Not long ago, the term ocular surface squamous neoplasia (OSSN) was used to include everything from simple dysplasia to carcinoma in situ to invasive squamous cell carcinoma.1 Before the umbrella term was coined, most corneal specialists labeled the disorders as conjunctival intraepithelial neoplasia, but "that term emphasized that the lesions were pre-cancer," said Shahzad I. Mian, M.D., associate professor, ophthalmology and visual sciences, Kellogg Eye Center, University of Michigan Medical School, Ann Arbor. "The advantage of having the simpler umbrella term is that people can use it more frequently and don't necessarily have to rely on histopathology as a clinical diagnosis."
The new terminology covers everything from mild to moderate to invasive, said Carol L. Karp, M.D., professor of clinical ophthalmology, Bascom Palmer Eye Institute, University of Miami Miller School of Medicine. "It encompasses the spectrum of squamous neoplasia that affects the conjunctiva." Prevalence is increasing, and OSSN is "the most common non-pigmented ocular tumor" diagnosed today, she said, but it's still rare.
OSSN has a rather low incidence (reported as high as 3.5 per 100,000 in areas closer to the equator and as low as 0.02 per 100,000 in areas farther from the equator). "A lot of patients will have common sun-related lesions, like pterygia," Dr. Karp said, "but OSSN is malignant." Most OSSN lesions are found around the limbus with prominent feeder blood vessels and a leukoplakia with a keratin plaque covering the lesion, said Dr. Mian. These lesions can also be gelatinous and may be on the cornea with an opaque look, Dr. Karp added.
Staining with rose bengal can be helpful in delineating a central lesion, she said. In her southern Florida location, she's even seen lesions that appear on the tarsal conjunctiva. Risk factors for OSSN include exposure to sunlight, fair skin/pale iris, human papilloma virus and HIV, cigarette smoking, chronic contact lens use, and chronic inflammation.
"There are non-invasive ways to diagnose OSSN," Dr. Karp said, among them impression cytology, ultra-high resolution optical coherence tomography, and confocal microscopy. The gold standard, however, is biopsy, she said.
"Bottom line—if you're unsure if it's OSSN or not, biopsy and send out for analysis," she said.
The risk of recurrence depends largely on the tumor type, size, and initial therapy, according to Yousef and Finger,2 with rates reported as low as 0% for T1- and T2-staged tumors to 50% for T4-staged tumors. The two also recommended treatment strategies be affected by tumor staging at presentation.
Treatment possibilities
Treatments for OSSN include topical medications such as mitomycin-C (MMC), 5-fluorouracil (5-FU), interferon, radiotherapy, or surgery. Traditionally, the treatment has been surgical excision, which can result in a "5-10% recurrence rate," Dr. Karp said. "While it works well in the majority of cases, extensive excisions carry the risk of limbal stem cell deficiency, scarring, and double vision." In her approach to treatment, she always offers both surgery and medical options. Surgery is best when the lesion is localized, the diagnosis is in question, the patient will not/can not put in drops, or the patient does not have the funds for the medications. Medical treatment is preferred in diffuse disease where it is difficult to tell where the surgical borders of the lesion are, in cases of recurrent OSSN, and in large or annular tumors where surgical removal could lead to limbal stem cell deficiency, or in patients who simply prefer not to undergo a procedure. "Topical medication has the benefit that it can treat the subclinical, invisible disease," Dr. Karp said. She recommended interferon alpha 2b, 5-FU, or MMC to treat these squamous lesions. These medications are off label, she said. If the patient is compliant and willing to use drops continuously for several months, her first line of medical treatment is interferon, 1 million IU/ml four times daily. It usually needs to be used for at least 3 months. "I like it because it is well tolerated, effective in most cases, and gentle," Dr. Karp said. If this does not work, she also uses MMC 0.02% or 0.04% four times daily for 1 week, then off until the eye recovers. MMC is very toxic and needs to be cycled. 5-FU 1% is another option she utilizes. This is also cycled, and she uses it four times daily for a week, like MMC, and then gives the eye the rest of the month to recover. MMC and 5-FU usually require three or more cycles and can be quite unpleasant.
Dr. Mian prefers to excise the lesion, using a double cryosurgery freeze-thaw technique to prevent recurrence, and opts for adjunctive therapy including topical chemo, MMC, and interferon. "Interferon alpha drops are much better tolerated in the eye [than MMC]," he said. MMC can cause epithelial toxicity, reactive conjunctivitis, and photophobia, which is why Dr. Karp has dubbed it the "devil drop." She notes that 5-FU is another topical drop option and calls it the "assistant devil drop." Interferon alpha 2b? "That's the angel drop," she said, but its downside is that it has to be used continuously for 3-4 months. In some cases, however, interferon can be injected anywhere from once to three times weekly. Intralesion interferon "doesn't need to be compounded and ensures patient compliance," she said. It does, however, give side effects of a "flu-like" feeling for several hours after the injection.
Local chemotherapy of MMC or 5-FU involves 1 week on, 1 week off, to give the conjunctiva time to heal, Dr. Mian noted. "If patients can tolerate the combination, the one on/one off schedule will let the tumor resolve faster, but if patients can't tolerate the drops, we'll give them a longer break in between dosing," he said. For ophthalmologists who don't often see these kinds of lesions, "don't ignore these when you see them," Dr. Mian said. "If we diagnose and treat these lesions early, we can achieve a complete cure rate in most patients."
References
1. Lee GA and Hirst LW. Ocular surface squamous neoplasia. Surv Ophthalmol. 1995;39(6):429-50.
2. Yousef YA, Finger PT. Squamous carcinoma and dysplasia of the conjunctiva and cornea: an analysis of 101 cases. Ophthalmology. 2012;119(2): 233-40. Epub 2011 Dec 20.
Editors' note: Drs. Karp and Mian have no financial interests related to this article.
Contact information
Karp: 305-326-6156, ckarp@med.miami.edu
Mian: 734-615-5476, smian@med.umich.edu
Treating ocular surface squamous neoplasia
--------------------------------------------------------------------------------
by Michelle Dalton EyeWorld Contributing Editor
Ocular surface squamous neoplasia (OSSN) is not a common condition but is one that all clinicians need to be able to recognize. An early diagnosis with a small lesion results in a very good prognosis. However, a delay in diagnosis can lead to a lesion that involves a large area of epithelium including a significant amount of the limbal stem cells and conjunctival. Treating these larger lesions is more difficult and has a higher recurrence rate. All clinicians should be aware of the clinical findings of OSSN: irregular, thickened limbal, corneal and conjunctival epithelium, and neovascularization. The abnormal epithelium typically arises from the limbus and can progress centrally over the cornea or posteriorly over the conjunctiva or in both directions. An atypical "pterygium" in an elderly patient should alert one to the diagnosis of OSSN.
Many new adjunct treatments are now available to reduce the recurrence and avoid the problem of multiple excisions in those cases of recurrence. Mitomycin-C (MMC), 5-fluorouracil (5-FU), and interferon alpha 2b are all adjunctive treatment choices in addition to the standard surgical resection and cryotherapy. In this issue's "Cornea corner of the world," Carol L. Karp, M.D., and Shahzad I. Mian, M.D., share their insights into the management of OSSN.
Edward J. Holland, M.D., cornea editor
A gelatinous-appearing ocular surface squamous neoplasia
Ocular surface squamous neoplasia in an HIV-positive patient. Note feeder vessels and both papillary and leukoplakic features of the lesion Source (all): Carol L. Karp, M.D.
This disease rarely metastasizes, but it can cause severe tissue destruction
Not long ago, the term ocular surface squamous neoplasia (OSSN) was used to include everything from simple dysplasia to carcinoma in situ to invasive squamous cell carcinoma.1 Before the umbrella term was coined, most corneal specialists labeled the disorders as conjunctival intraepithelial neoplasia, but "that term emphasized that the lesions were pre-cancer," said Shahzad I. Mian, M.D., associate professor, ophthalmology and visual sciences, Kellogg Eye Center, University of Michigan Medical School, Ann Arbor. "The advantage of having the simpler umbrella term is that people can use it more frequently and don't necessarily have to rely on histopathology as a clinical diagnosis."
The new terminology covers everything from mild to moderate to invasive, said Carol L. Karp, M.D., professor of clinical ophthalmology, Bascom Palmer Eye Institute, University of Miami Miller School of Medicine. "It encompasses the spectrum of squamous neoplasia that affects the conjunctiva." Prevalence is increasing, and OSSN is "the most common non-pigmented ocular tumor" diagnosed today, she said, but it's still rare.
OSSN has a rather low incidence (reported as high as 3.5 per 100,000 in areas closer to the equator and as low as 0.02 per 100,000 in areas farther from the equator). "A lot of patients will have common sun-related lesions, like pterygia," Dr. Karp said, "but OSSN is malignant." Most OSSN lesions are found around the limbus with prominent feeder blood vessels and a leukoplakia with a keratin plaque covering the lesion, said Dr. Mian. These lesions can also be gelatinous and may be on the cornea with an opaque look, Dr. Karp added.
Staining with rose bengal can be helpful in delineating a central lesion, she said. In her southern Florida location, she's even seen lesions that appear on the tarsal conjunctiva. Risk factors for OSSN include exposure to sunlight, fair skin/pale iris, human papilloma virus and HIV, cigarette smoking, chronic contact lens use, and chronic inflammation.
"There are non-invasive ways to diagnose OSSN," Dr. Karp said, among them impression cytology, ultra-high resolution optical coherence tomography, and confocal microscopy. The gold standard, however, is biopsy, she said.
"Bottom line—if you're unsure if it's OSSN or not, biopsy and send out for analysis," she said.
The risk of recurrence depends largely on the tumor type, size, and initial therapy, according to Yousef and Finger,2 with rates reported as low as 0% for T1- and T2-staged tumors to 50% for T4-staged tumors. The two also recommended treatment strategies be affected by tumor staging at presentation.
Treatment possibilities
Treatments for OSSN include topical medications such as mitomycin-C (MMC), 5-fluorouracil (5-FU), interferon, radiotherapy, or surgery. Traditionally, the treatment has been surgical excision, which can result in a "5-10% recurrence rate," Dr. Karp said. "While it works well in the majority of cases, extensive excisions carry the risk of limbal stem cell deficiency, scarring, and double vision." In her approach to treatment, she always offers both surgery and medical options. Surgery is best when the lesion is localized, the diagnosis is in question, the patient will not/can not put in drops, or the patient does not have the funds for the medications. Medical treatment is preferred in diffuse disease where it is difficult to tell where the surgical borders of the lesion are, in cases of recurrent OSSN, and in large or annular tumors where surgical removal could lead to limbal stem cell deficiency, or in patients who simply prefer not to undergo a procedure. "Topical medication has the benefit that it can treat the subclinical, invisible disease," Dr. Karp said. She recommended interferon alpha 2b, 5-FU, or MMC to treat these squamous lesions. These medications are off label, she said. If the patient is compliant and willing to use drops continuously for several months, her first line of medical treatment is interferon, 1 million IU/ml four times daily. It usually needs to be used for at least 3 months. "I like it because it is well tolerated, effective in most cases, and gentle," Dr. Karp said. If this does not work, she also uses MMC 0.02% or 0.04% four times daily for 1 week, then off until the eye recovers. MMC is very toxic and needs to be cycled. 5-FU 1% is another option she utilizes. This is also cycled, and she uses it four times daily for a week, like MMC, and then gives the eye the rest of the month to recover. MMC and 5-FU usually require three or more cycles and can be quite unpleasant.
Dr. Mian prefers to excise the lesion, using a double cryosurgery freeze-thaw technique to prevent recurrence, and opts for adjunctive therapy including topical chemo, MMC, and interferon. "Interferon alpha drops are much better tolerated in the eye [than MMC]," he said. MMC can cause epithelial toxicity, reactive conjunctivitis, and photophobia, which is why Dr. Karp has dubbed it the "devil drop." She notes that 5-FU is another topical drop option and calls it the "assistant devil drop." Interferon alpha 2b? "That's the angel drop," she said, but its downside is that it has to be used continuously for 3-4 months. In some cases, however, interferon can be injected anywhere from once to three times weekly. Intralesion interferon "doesn't need to be compounded and ensures patient compliance," she said. It does, however, give side effects of a "flu-like" feeling for several hours after the injection.
Local chemotherapy of MMC or 5-FU involves 1 week on, 1 week off, to give the conjunctiva time to heal, Dr. Mian noted. "If patients can tolerate the combination, the one on/one off schedule will let the tumor resolve faster, but if patients can't tolerate the drops, we'll give them a longer break in between dosing," he said. For ophthalmologists who don't often see these kinds of lesions, "don't ignore these when you see them," Dr. Mian said. "If we diagnose and treat these lesions early, we can achieve a complete cure rate in most patients."
References
1. Lee GA and Hirst LW. Ocular surface squamous neoplasia. Surv Ophthalmol. 1995;39(6):429-50.
2. Yousef YA, Finger PT. Squamous carcinoma and dysplasia of the conjunctiva and cornea: an analysis of 101 cases. Ophthalmology. 2012;119(2): 233-40. Epub 2011 Dec 20.
Editors' note: Drs. Karp and Mian have no financial interests related to this article.
Contact information
Karp: 305-326-6156, ckarp@med.miami.edu
Mian: 734-615-5476, smian@med.umich.edu





留言
張貼留言